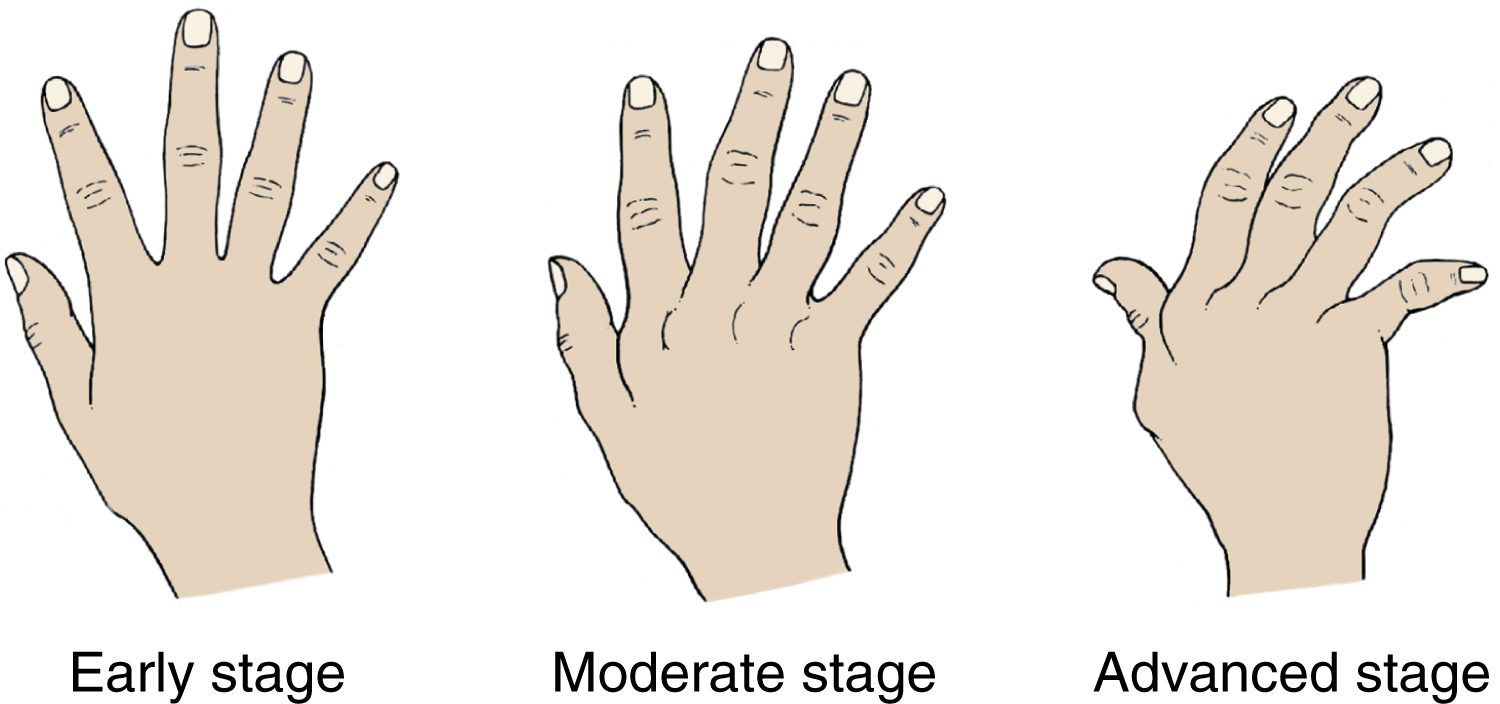
rheumatoid arthritis (RA) [Gk, rheuma, flux, eidos, form, arthron, joint, itis, inflammation] , a chronic, inflammatory, destructive, and sometimes deforming collagen disease that has an autoimmune component. It is characterized by symmetric inflammation of synovial membranes and increased synovial exudate, leading to thickening of the membranes and swelling of the joints. Rheumatoid arthritis usually first appears when patients, most often women, are between 36 and 50 years of age. The course of the disease is variable but is most frequently marked by alternating periods of remission and exacerbation. Also called arthritis deformans, atrophic arthritis. See also ankylosing spondylitis, juvenile rheumatoid arthritis. ▪ OBSERVATIONS: The medical diagnosis and prognosis of rheumatoid arthritis are based on a variety of clinical and laboratory findings. The disease may first be present with fatigue, weakness, poor appetite, low-grade fever, anemia, and an increased erythrocyte sedimentation rate. The diagnostic criteria listed by the American Rheumatism Association include morning stiffness, joint pain or tenderness, swelling of at least two joints, subcutaneous nodules (called arthritic nodules and usually found at pressure points such as the elbows), structural changes in joints seen on x-ray film, a positive rheumatoid factor agglutination test, decreased precipitation of mucin from synovial fluid, and characteristic histological changes on pathological examination of the fluid. Higher titers of rheumatoid factor are correlated with more severe forms of the disease, especially forms with extraarticular manifestations, such as cardiac involvement, vasculitis, pulmonary disease, and proteinuria. There may also be a thickening of synovial membranes, called pannus formation. In long-term, severe, chronic rheumatoid arthritis, Felty’s syndrome may be present. Rheumatoid arthritis is not always progressive, deforming, or debilitating; most patients may continue in their jobs. ▪ INTERVENTIONS: Treatment includes sufficient rest, range-of-motion exercises to maintain joint function, medication for the relief of pain and reduction of inflammation, orthopedic intervention to prevent or correct deformities, proper nutrition, and weight loss, if necessary. Salicylates are usually given. If improvement is not achieved, other antiinflammatory agents may be used, such as indomethacin, phenylbutazone, antimalarials, gold salts, or some antineoplastic drugs. Corticosteroids are prescribed with caution because of their side effects, including gastric ulcer, adrenal suppression, and osteoporosis. Disease-modifying antirheumatic drugs (DMARDs) and biologic response modifiers can slow the progression of the disease and prevent permanent damage to the joints and other tissues. Other treatments, including diathermy, ultrasound, warm paraffin applications, underwater exercise, and applications of heat, are occasionally used. ▪ PATIENT CARE CONSIDERATIONS: The health care team monitors drug treatment and notes its effects. Health care providers also encourage the patient to get sufficient sleep and to rest both small and weight-bearing joints. The involvement of occupational and physical therapy is important to ensure that measures to protect the joints are implemented. The most effective use of heat or cold; instruction in muscle-strengthening exercises and in methods for easing pain and preventing deformities, such as the proper use of pillows, splints, or molds; and offers of emotional support should also be addressed.