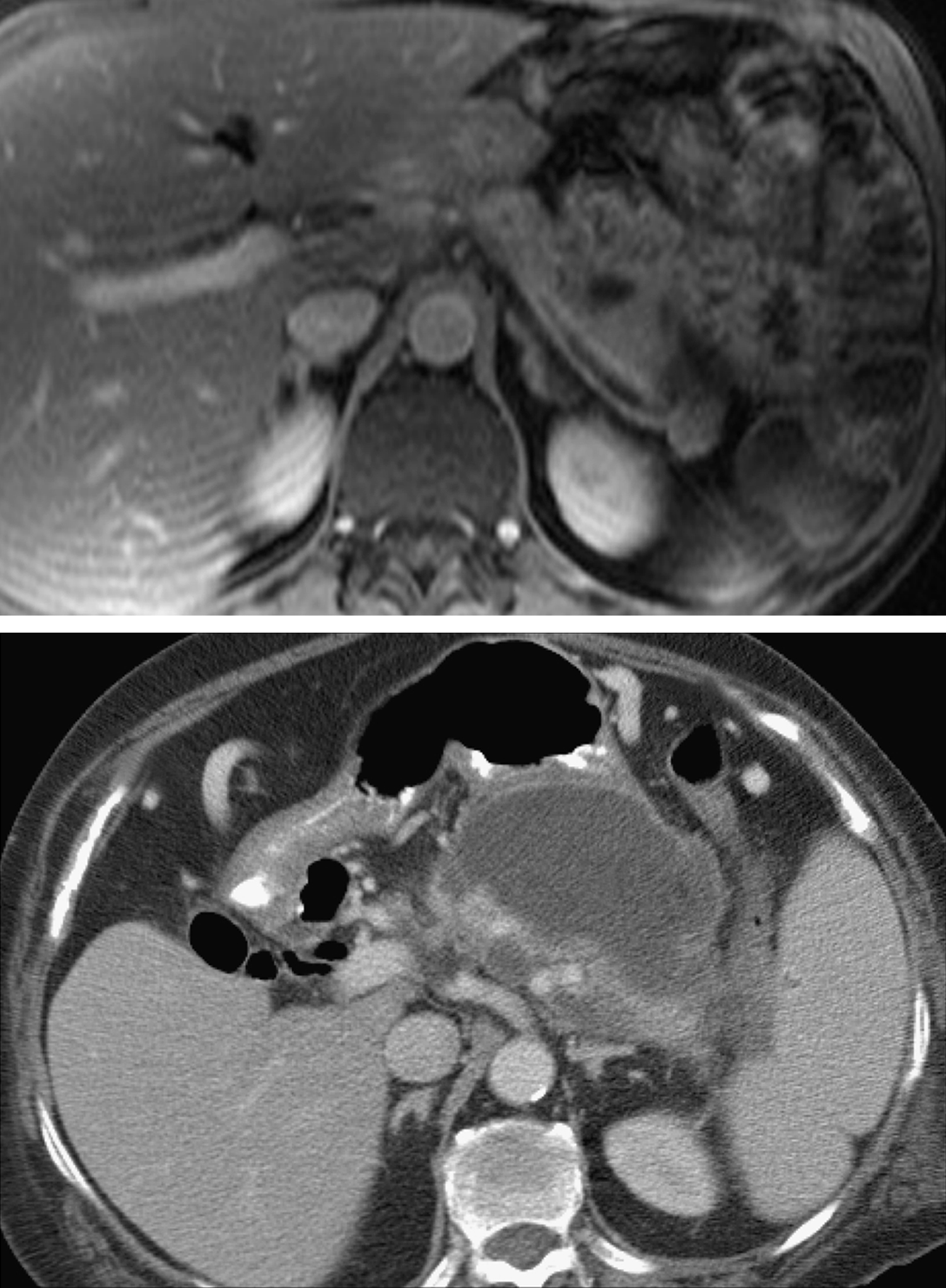
pancreatitis /pan′krē·ətī″tis/ [Gk, pan + kreas + itis, inflammation] , an inflammatory condition of the pancreas that may be acute or chronic. Acute pancreatitis is generally the result of damage to the biliary tract, as by alcohol, trauma, infectious disease, or certain drugs. It is characterized by severe abdominal pain (generally epigastric or upper left) radiating to the back, fever, anorexia, nausea, and vomiting. There may be jaundice if the common bile duct is obstructed. The development of pseudocysts or abscesses in pancreatic tissue is a serious complication. Treatment includes nasogastric suction to remove gastric secretions. To prevent any stimulation of the pancreas, nothing is given by mouth. The client may be given antacids to decrease the acid, which stimulates the pancreas. IV fluids and electrolytes are administered, and nonmorphine derivatives are given to relieve pain. The causes of chronic pancreatitis are similar to those of the acute form. When the cause is alcohol abuse, there may be calcification and scarring of the smaller pancreatic ducts. Abdominal pain, nausea, and vomiting occur, as well as steatorrhea and creatorrhea, caused by the diminished output of pancreatic enzymes. Pancreatic insulin production may be diminished, and diabetes mellitus develops in some patients. Treatment includes analgesics for pain and subtotal pancreatectomy when pain is intractable. A pancreatic extract is given orally to replace the missing enzymes; vitamin supplements are essential; and calcium supplements may be needed. Both forms of pancreatitis are diagnosed by history, physical examination, radiological studies, endoscopy, and laboratory analysis of the amount of pancreatic enzymes in the blood.