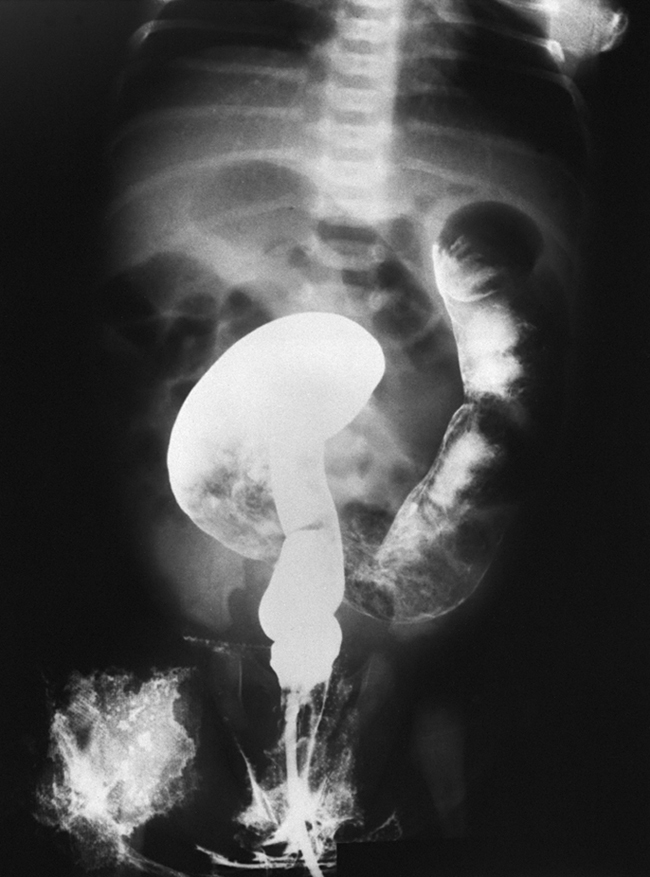
Hirschsprung’s disease /hirsh″spro͝ongz/ [Harald Hirschsprung, Danish physician, 1830–1916] , the congenital absence of autonomic ganglia in the smooth muscle wall of the distal part of the colon, which causes poor or absent peristalsis in the involved segment of colon, accumulation of feces, and dilation of the bowel (megacolon). Symptoms include intermittent vomiting, diarrhea, and constipation. The abdomen may become distended to several times its normal size. The condition is usually diagnosed in infancy, but it may not be recognized until much later in childhood, when anorexia, lack of urge to defecate, distention of the abdomen, and poor health occur. Diagnosis is confirmed by barium enema; biopsy of the affected tissue shows the absence of ganglia. Surgical repair in early childhood is usually successful. A temporary colostomy is performed, and the aganglionic portion of the bowel is resected. The colostomy is almost always reversed a few months later. Also called aganglionic megacolon, congenital megacolon. ▪ OBSERVATIONS: Manifestation patterns vary according to the length of the affected bowel. Neonates may be asymptomatic during the first few months of life. In a complete obstruction, signs include delayed passage of meconium, obstipation, massive abdominal distention, refusal to feed, and bilious vomiting. In a partial obstruction there are cycles of constipation and diarrhea with thin ribbon-like stools, intermittent vomiting, abdominal distention, and possible failure to thrive. If the condition goes undiagnosed until childhood, there are signs of anorexia, abdominal distention, lack of urge to defecate, and general poor health. Diagnosis is made through observation of clinical signs of obstruction and barium enema results that reveal narrowing of the colon distal to obstruction and enlargement of the colon proximal to the obstruction. Diagnosis is confirmed by a rectal suction biopsy that reveals no evidence of ganglion cells. Enterocolitis or toxic megacolon is the most serious complication and is marked by sudden onset fever, abdominal distention, and explosive bloody diarrhea. Enterocolitis causes death in about 20% of the cases. ▪ INTERVENTIONS: The treatment is relief of the obstruction by one of several procedures, including a Soave endorectal pull through, a Duhamel procedure to create a neorectum, a Swenson’s procedure to resect the aganglionic segment, a laparoscopic pull-through procedure, or a transanal endorectal coloanal anastomosis. A myectomy may be performed if only the anal segment is involved. A myectomy/myotomy may be indicated if the entire intestine is involved. A temporary ostomy is created to relieve obstruction and to promote healing after surgery. Antiinfectives are used to treat or prevent infection. Analgesics are used to control pain, and antiemetics are used for nausea and vomiting. ▪ PATIENT CARE CONSIDERATIONS: Acute care focuses on routine preoperative and postoperative care, including saline enemas to prep the bowel for surgery, comfort measures, IV hydration, I and O, abdominal measurements, support and reassurance to child and family, colostomy care, and wound care. Instruction is needed for care and cleaning of the colostomy, and a home health care referral will help establish continuity of such care. Caregivers should be educated to expect continuing soiling incidents after surgery. Genetic counseling is needed for the parents.