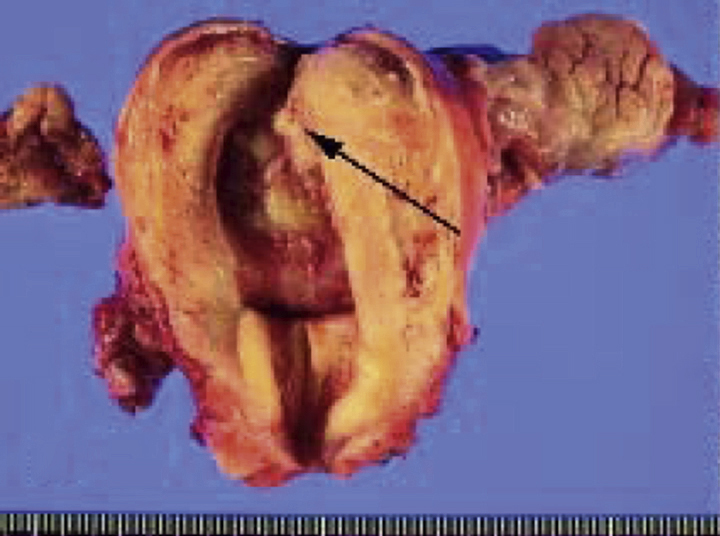
endometrial cancer, a carcinoma of the endometrium of the uterus. It is the most prevalent gynecological malignancy, most often occurring in the fifth or sixth decade of life. Although the cause of endometrial cancer is not clear, some of the risk factors associated with an increased incidence of the disease are a medical history of infertility, anovulation, late menopause (52 years), administration of unopposed exogenous estrogen, uterine polyps, and a combination of diabetes, hypertension, and obesity. Adenocarcinomas constitute roughly 90% of all endometrial tumors; the remaining 10% comprise mixed carcinomas, sarcomas, and benign adenoacanthomas. ▪ OBSERVATIONS: Abnormal vaginal bleeding, especially in a postmenopausal woman, is the cardinal symptom. Lower abdominal and low back pain may also be present; a large, boggy uterus is often a sign of advanced disease. Fewer than half the patients with endometrial cancer have a positive finding on Papanicolaou’s (Pap) test of the cervix and vagina because the tumor cells rarely exfoliate in early stages of the lesion. A Pap test of cells removed from the endometrium obtained from jet washings of the uterine cavity provides more accurate data. Vacuum curettage is also used to extract endometrial cells for study, but the diagnostic technique most frequently recommended is dilation and curettage, in which each section of the uterus is examined and curetted for biopsy specimens. ▪ INTERVENTIONS: Endometrial lesions may spread to the cervix but rarely invade the vagina. They metastasize to the broad ligaments, fallopian tubes, and ovaries so frequently that bilateral salpingo-oophorectomy with abdominal hysterectomy is the usual treatment. Radiotherapy is usually administered before and after surgery. High doses of a progestogen may be prescribed for palliation in advanced or inoperable cases. Chemotherapy may also be used. ▪ PATIENT CARE CONSIDERATIONS: Survival rates are high if the disease is identified at an early stage.