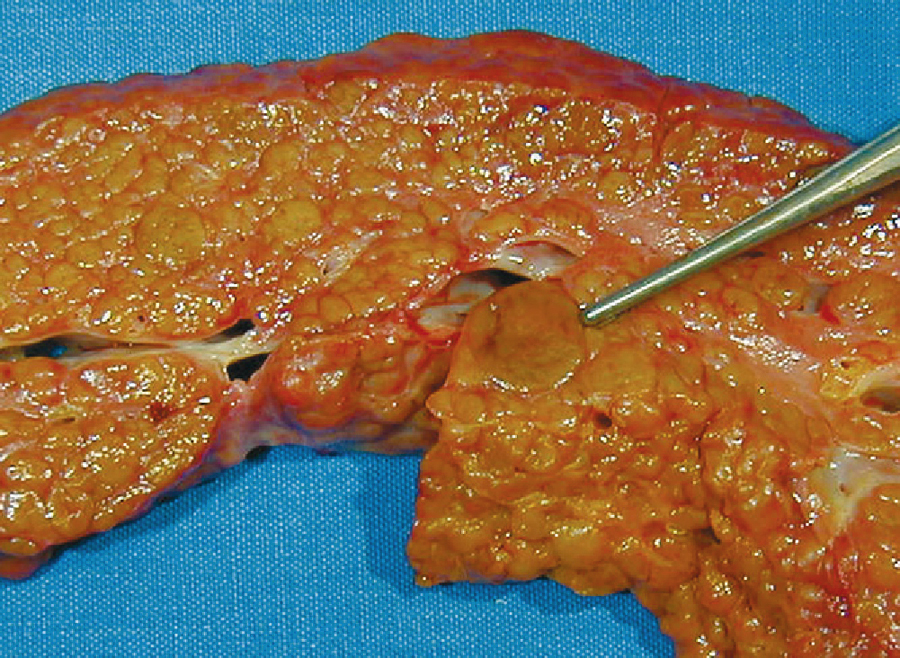
cirrhosis /sirō″sis/ [Gk, kirrhos, yellow-orange, osis, condition] , a chronic degenerative disease of the liver in which the lobes are covered with fibrous tissue, the parenchyma degenerates, and the lobules are infiltrated with fat. Gluconeogenesis, detoxification of drugs and alcohol, bilirubin metabolism, vitamin absorption, GI function, hormonal metabolism, and other functions of the liver deteriorate. Blood flow through the liver is obstructed, causing back pressure and leading to portal hypertension and esophageal varices. Unless the cause of the disease is removed, hepatic coma, GI hemorrhage, and kidney failure may occur. Cirrhosis is most commonly the result of chronic alcohol abuse; other causes include nutritional deprivation, hepatitis, and cardiac problems. ▪ OBSERVATIONS: Cirrhosis is often asymptomatic in early disease or may manifest as abdominal pain, diarrhea, nausea, vomiting, fatigue, and fever. As the disease progresses, manifestations such as chronic dyspepsia, constipation, anorexia, weight loss, pruritus, easy bruising, bleeding gums, nosebleeds, upper gastrointestinal bleeding, and enlarged liver are seen. Late disease is accompanied by telangiectasis, spider angiomas, enlarged breasts, testicular atrophy, jaundice, impotence, enlarged spleen, depression, abdominal vein distention, ascites, encephalopathy, and peripheral neuropathy. Diagnostic tests include abnormal liver function studies, including elevations in alkaline phosphatase, aminotransferase, and alanine aminotransferase. A CBC may show evidence of anemia, leukopenia, or thrombocytopenia. Protein metabolism tests show decreased total protein, decreased albumin, and increased globulin. Cholesterol levels are decreased as a result of abnormalities in fat metabolism. Prothrombin time is prolonged, and bilirubin metabolism is abnormal. Blood glucose may be reduced. Ultrasonography is used to reveal hepatosplenomegaly and enlarged portal veins. Liver scans show reduced liver uptake. Liver biopsy will show definitive histological changes in the liver cells and reveal altered structure in the lobes. ▪ INTERVENTIONS: The first step is elimination of toxic agents, such as alcohol or drugs. Therapy is aimed at liver cell regeneration and the prevention or treatment of symptoms. This includes rest to reduce metabolic demands on the liver; a high-calorie, high-protein (unless hepatic encephalopathy is present), high-carbohydrate, and low-fat, low-sodium diet; diuretics to reduce edema; digestants to promote fat digestion; supplemental vitamins; and stool softeners. Ascites may be treated with abdominal paracentesis or peritoneovenous shunt. Esophageal varices may be treated by using blood and blood products, gastric lavage, or esophageal balloon to stem bleeding. Variceal sclerosis may be performed via endoscopy to eliminate the varicosities. A portal systemic shunt may be surgically placed to treat resistant esophageal varices. A transjugular intrahepatic portosystemic shunt may be used to divert portal blood from the liver to relieve portal hypertension. Renal dialysis is used to treat renal failure. Hepatic encephalopathy is managed by reducing ammonia formation through reduced protein intake, administering lactulose to decrease pH in the intestines, and administering antibiotics to reduce bacterial flora in the colon. Liver transplantation may be the only hope for those with advanced disease. ▪ PATIENT CARE CONSIDERATIONS: Care for individuals with acute disease is multifaceted, complex, and dictated by the stage of the disease and presenting symptomatology. The focus is on strength conservation. This includes balancing rest and activity and correcting nutritional imbalances. Edema and ascites produce itching and impaired skin integrity. Skin care requires careful diligence to prevent excoriation and breakdown. Ascites can also produce shortness of breath from pressure placed on the diaphragm. Sensory perception may be decreased secondary to peripheral neuropathy. This places the individual at increased risk for injury and requires the implementation of injury prevention protocols. Infection control measures should also be in effect to reduce the possibility of infection from environmental pathogens in these susceptible individuals. Careful monitoring is needed to spot early signs of life-threatening complications, such as hepatic encephalopathy or esophageal bleeding. In the individual with hepatic encephalopathy, the focus is on monitoring systems affected by increased ammonia levels and assessing whether levels are effectively being reduced. Adequate hydration must be maintained with careful monitoring for fluid and electrolyte and acid-base imbalances, reduction of protein, prevention of constipation, and strict bed rest. Chronic care focuses on education. Individuals need to understand that this disease is chronic in nature and requires continuous care to reduce or prevent serious complications. Prompt treatment needs to be sought at any sign of complication. Instruction is needed about diet, medication use and restrictions, skin care, infection protection, and importance of complete alcohol abstinence. Referrals may be made to substance abuse programs and community or home health care agencies.