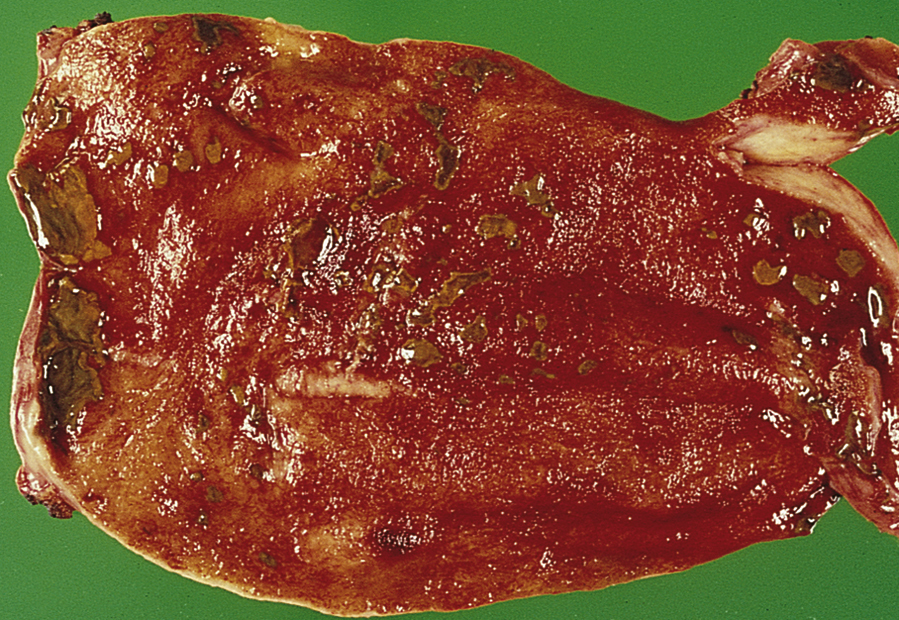
cholecystitis /kō′lisistī″tis/ [Gk, chole + kystis, bag, itis, inflammation] , acute or chronic inflammation of the gallbladder. Acute cholecystitis is usually caused by a gallstone that cannot pass through the cystic duct. Pain is felt in the right upper quadrant of the abdomen, accompanied by nausea, vomiting, eructation, and flatulence. The patient may exhibit a positive Murphy’s sign. Diagnosis is usually made with ultrasound. Surgery is the preferred mode of treatment. Chronic cholecystitis, the more common type, has an insidious onset. Pain, often felt at night, may follow a fatty meal. Complications include biliary calculi, pancreatitis, and carcinoma of the gallbladder. Again surgery is the preferred treatment. See also biliary calculus, cholecystectomy, cholelithiasis. ▪ OBSERVATIONS: Common manifestations for cholecystitis may range from indigestion to moderate to severe abdominal or shoulder pain accompanied by fever and jaundice. Symptoms for acute cholecystitis include colicky pain in right upper quadrant and right lower scapula, nausea and vomiting, and low-grade fever. Manifestations indicative of chronic cholecystitis include anorexia, flatulence, nausea, fat intolerance, episodic or diffuse abdominal pain, and heartburn. The gallbladder may be palpable, and palpation of right upper quadrant may elicit tenderness and stoppage of inspiration (Murphy’s sign). History may show ingestion of a large fatty meal before onset of pain. Ultrasonography is often performed initially to visualize gallstones. A nuclear imaging (hepatobiliary iminodiacetic acid scan) is useful in diagnosing acute cholecystitis. Necrosis and perforation of the gallbladder with generalized peritonitis, cholangitis with or without septic shock, pancreatitis, biliary cirrhosis, and bowel obstruction with perforation and peritonitis are all complications of biliary disease. ▪ INTERVENTIONS: Conservative treatment of a cholecystitis attack includes control of pain, prevention of infection, and maintenance of fluid and electrolyte balance. Gastric decompression to reduce stimulation of the gallbladder may be indicated for control of severe nausea and vomiting. Antiinfective drugs are used to prevent infection, analgesics to treat pain, anticholinergics to reduce secretions, and antispasmodics to reduce smooth muscle spasms. Fat soluble vitamins and bile salts may also be prescribed. Laparoscopic cholecystectomy may be indicated to remove the gallbladder in acute disease. Endoscopic balloon or basket procedures may be used to remove stones. An endoscope retrograde cholangiopancreatography with or without stent placements and sphincterotomy may be used to extract ductal stones. Pulverization of stones by lithotripsy or dissolution of stones by oral ursodiol or methyl terbutyl instilled into gallbladder may also be used. ▪ PATIENT CARE CONSIDERATIONS: Acute care is directed toward pain relief and fluid and electrolyte management. Preoperative care includes education about the surgical experience and reduction of anxiety about impending surgery. Postoperative care focuses on pain management, adequate ventilation, and prevention of postsurgical complications, such as bleeding or infection of surgical site. Education for those with an intact gallbladder includes instruction in a low-fat diet, institution of a consistent exercise program, and maintenance of normal weight. Any weight loss needs to be done slowly (1 to 2 lb a week) to prevent sludgy bile. If stones have been removed, the individual needs to understand that stones can recur and that medical follow-up is necessary.