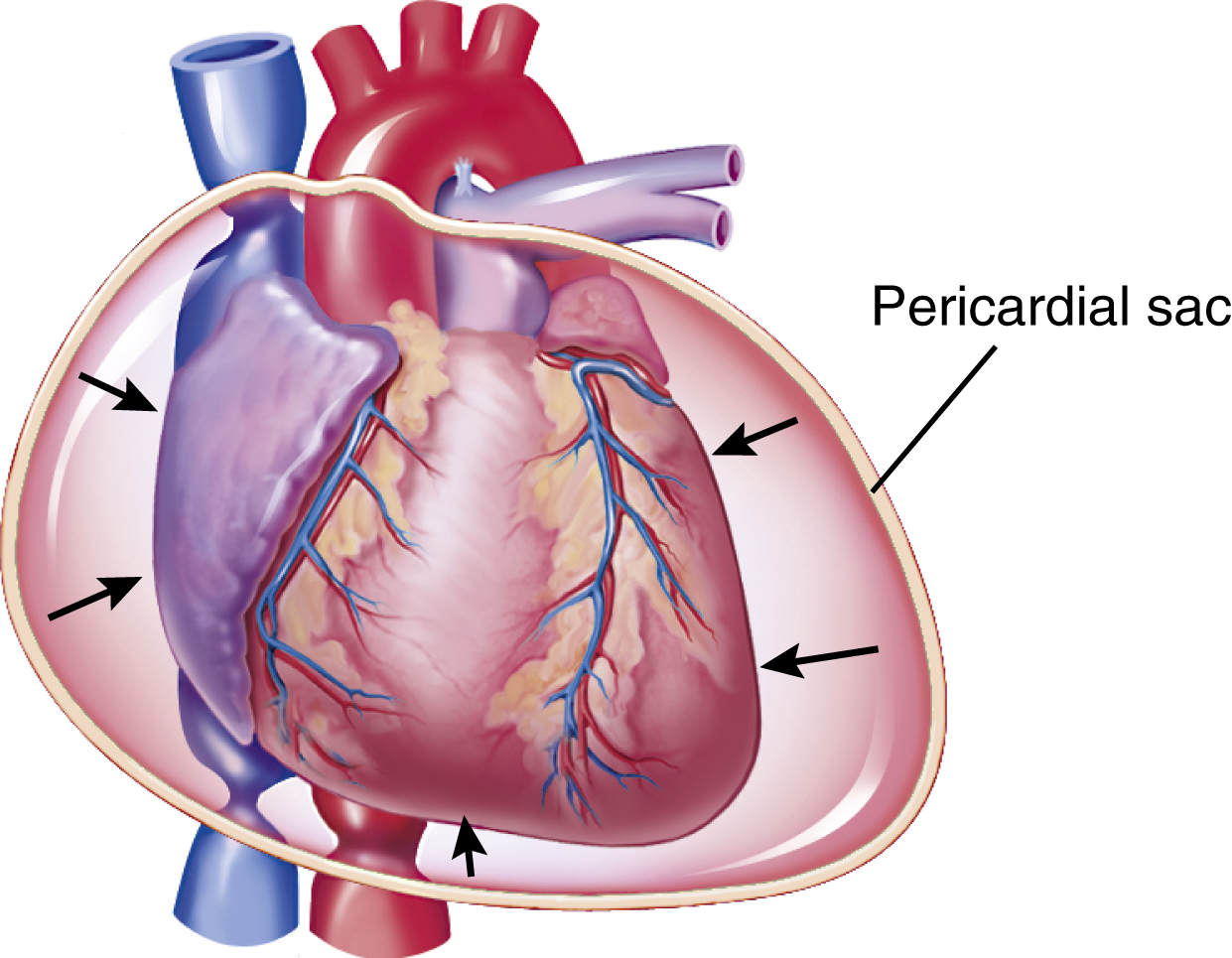
cardiac tamponade /tam′pənäd″/ , compression of the heart produced by the accumulation of blood or other fluid in the pericardial sac. Also called cardiac compression, pericardial tamponade. ▪ OBSERVATIONS: Signs of cardiac tamponade may include distended neck veins, hypotension, decreased heart sounds, tachypnea, peripheral pulses that are weak or absent or that fall sharply during inspiration (pulsus paradoxus), reduced left atrial pressure, and pericardial friction rub. The patient, who is usually anxious and restless, may sit upright or lean forward, and the skin may be pale, dusky, or cyanotic. The electrocardiogram generally shows decreased cardiac voltage and may show electrical alternans, and the chest x-ray film may reveal an enlarged heart shadow (“water bottle” heart). ▪ INTERVENTIONS: The patient is maintained on bed rest; the head of the bed is elevated 45 degrees, and a defibrillator and emergency drugs are kept at the bedside. IV saline is the initial therapy of choice to maintain filling pressures in the heart. Blood pressure, respiration, apical pulse, and atrial and pulmonary wedge pressures are checked every 15 to 30 minutes. Auscultation for pulsus paradoxus is performed, and peripheral pulses are checked every 30 minutes. A 12-lead electrocardiogram is usually ordered, and the patient is placed on a cardiac monitor with the rhythm strip checked every hour. A Doppler echocardiogram is done initially and may be repeated a few days later. Cardiotonic and antiarrhythmic drugs are administered as ordered. Aspiration of the fluid in the pericardial sac (pericardiocentesis) is performed, and, if surgery is indicated, the patient is prepared for the procedure. In cases in which bleeding vessels are the cause of the tamponade, the vessels are ligated.