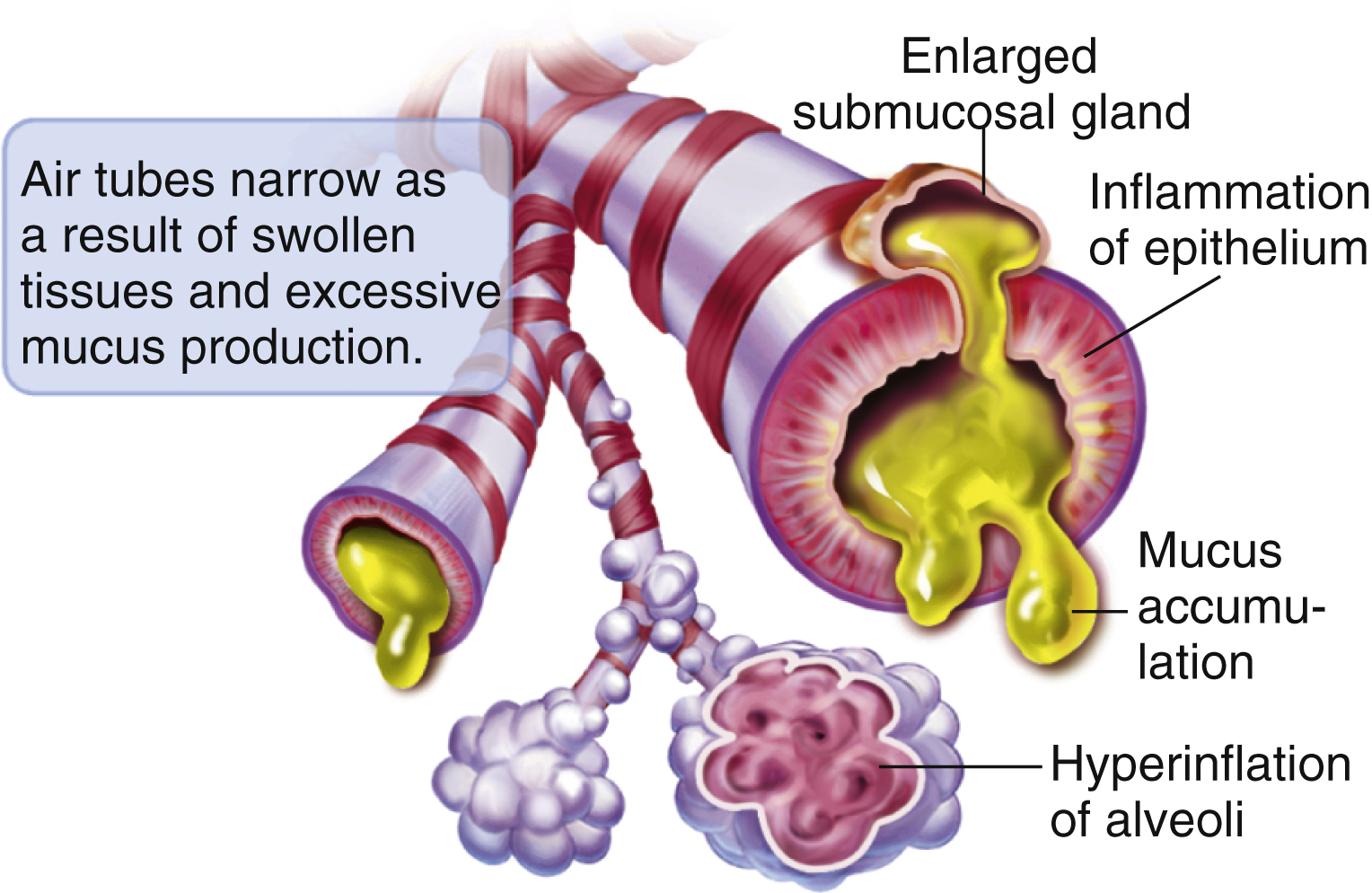
bronchitis /brongkī″tis/ [Gk, bronchos, windpipe, itis, inflammation] , acute or chronic inflammation of the mucous membranes of the tracheobronchial tree. Caused by the spread of upper respiratory viral or sometimes bacterial infections to the bronchi, it is often observed with or after childhood infections, such as measles, whooping cough, diphtheria, and typhoid fever. See also chronic bronchitis, chronic obstructive pulmonary disease, respiratory syncytial virus. ▪ OBSERVATIONS: Acute bronchitis is frequently preceded by an upper respiratory infection. The most common presenting sign is a dry, hacking cough that increasingly produces viscous mucus. Other symptoms include low-grade fever, substernal pain, and fatigue. Rhonchi and occasional wheezing may be heard when auscultating lungs. Diagnosis is usually made from the type of cough and sputum. Chest x-rays are taken to rule out other disorders. Arterial blood gases are monitored when the underlying chronic disease is present, and sputum is cultured for evidence of superimposed infection. Pneumonia is the most common complication. Acute respiratory failure occurs in some individuals with underlying pulmonary disease. Chronic bronchitis may be asymptomatic for years. A productive cough with copious mucopurulent sputum, peripheral cyanosis, and variable dyspnea are typical presenting signs. The cough becomes increasingly progressive and the sputum production more copious. Wheezing, tachypnea, and tachycardia may also be present. Several attacks per year are common. Chest x-rays reveal cardiac enlargement, congested lung fields, and thickened bronchial markings. Pulmonary function studies show increased residual volume and decreases in forced vital capacity and forced expiratory volume. PaO2 is decreased and PaCO2 increased on arterial blood gas results. Sputum cultures show presence of multiple microorganisms and neutrophils. Cor pulmonale, pulmonary hypertension, right ventricular hypertrophy, and respiratory failure are common complications seen in chronic bronchitis. ▪ INTERVENTIONS: Treatment for acute episodes include medications, such as inhaled bronchodilators for wheezing, expectorants for cough, and antipyretics for fever. Antiinfective drugs are used only with concomitant chronic obstructive pulmonary disease (COPD) or a superimposed infection. Adequate hydration and a vaporizer help liquefy secretions. Treatment for chronic bronchitis includes antiinfective drugs for infection, bronchodilators to reduce dyspnea, and corticosteroids to reduce inflammation. Chest physiotherapy is used to loosen secretions. Oxygenation is used for hypoxia. Health promotion in individuals with chronic disease include a consistent exercise program to improve ventilatory and cardiac function; smoking cessation programs and use of flu and pneumonia vaccines for prophylaxis. ▪ PATIENT CARE CONSIDERATIONS: The focus of care during acute episodes is supportive and includes rest, increased fluids, and steam vaporizer. Education plays a large role for those suffering from chronic bronchitis and includes information on the disease process; instruction on medication administration (schedule and use of spacer), home use of oxygen, chest physiotherapy program, effective coughing, exercise program, nutrition plan to decrease weight if indicated, smoking cessation if indicated, and proper use of respirators in workplace if exposed to respiratory irritants. Importance of long-term and consistent follow-up should be stressed.