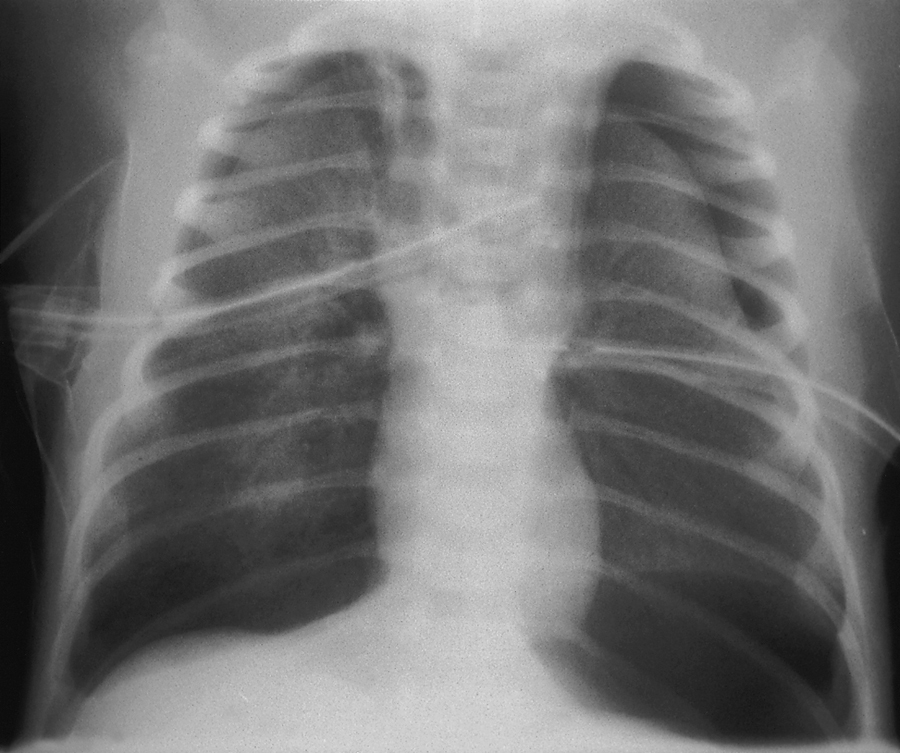
respiratory distress syndrome of the newborn (RDS), an acute lung disease of the newborn, characterized by airless alveoli, inelastic lungs, a respiration rate greater than 60 breaths per minute, nasal flaring, intercostal and subcostal retractions, grunting on expiration, and peripheral edema. The condition occurs most often in premature babies. It is caused by a deficiency of pulmonary surfactant, resulting in overdistended alveoli and at times hyaline membrane formation, alveolar hemorrhage, severe right-to-left shunting of blood, increased pulmonary resistance, decreased cardiac output, and severe hypoxemia. Treatment includes measures to correct shock, acidosis, and hypoxemia and use of continuous positive airway pressure to prevent alveolar collapse. Also called hyaline membrane, idiopathic respiratory distress syndrome. Compare adult respiratory distress syndrome. ▪ OBSERVATIONS: Signs and symptoms usually appear within 6 hours of birth and include rapid respirations, nostril flaring, expiratory grunting, chest retractions, labored breathing, frothing at lips, inspiratory crackles, cyanosis, and weak cry. These manifestations progress to apnea, flaccidity, unresponsiveness, mottling, peripheral edema, oliguria, hypotension, and bradycardia. Diagnosis is made by clinical exam, chest x-rays that display a diffuse granular pattern in bilateral lung fields indicating atelectasis, and bronchograms representing dilated air-filled bronchioles. Pulmonary function studies are run to differentiate a pulmonary from extrapulmonary illness. Blood gases are taken to determine the extent of respiratory function and acid-base imbalances. Possible complications include intraventricular hemorrhage, tension pneumothorax, retinopathy of prematurity, bronchopulmonary dysplasia, apnea, patent ductus arteriosus, congestive heart failure, neurological sequelae, necrotizing enterocolitis, pneumonia, sepsis, and/or death. ▪ INTERVENTIONS: Treatment is largely supportive. Exogenous surfactant is administered as soon as possible after birth and the infant is transported to the intensive care unit. Ventilation is started by continuous positive airway pressure. Warm, humidified oxygen therapy is used. Nutrition is managed by parenteral therapy (nipple and gavage feeding are contraindicated). Continued and aggressive laboratory monitoring of respiratory, circulatory, acid-base, and electrolyte status is performed. Blood transfusions may be necessary to replace blood lost during aggressive monitoring. Preventive measures are instituted with pregnant women by administering betamethasone injections to those mothers 24 to 48 hours before the delivery of any premature infant 24 to 34 weeks in gestation. ▪ PATIENT CARE CONSIDERATIONS: Acute nursing and respiratory care is focused on adequate ventilation, oxygenation, maintenance of fluid and nutrition, and prevention of complications. Positioning aids in ventilation; use of blanket rolls and warmers reduces heat loss and lowers oxygen and glucose consumption and metabolic requirements. Careful intake and output, daily weights, and hydration assessments are used to monitor fluids and nutrition. Care clustering helps provide rest between the multiple interventions, such as suctioning, blood sticks, arterial blood gas draws, medication administration, and assessments. Parental support and education about infant treatments and monitoring are necessary. Parents should be educated about the self-limiting nature of the disease. The need for long-term medical follow-up should be stressed to monitor for and detect potential neurological and respiratory sequelae.