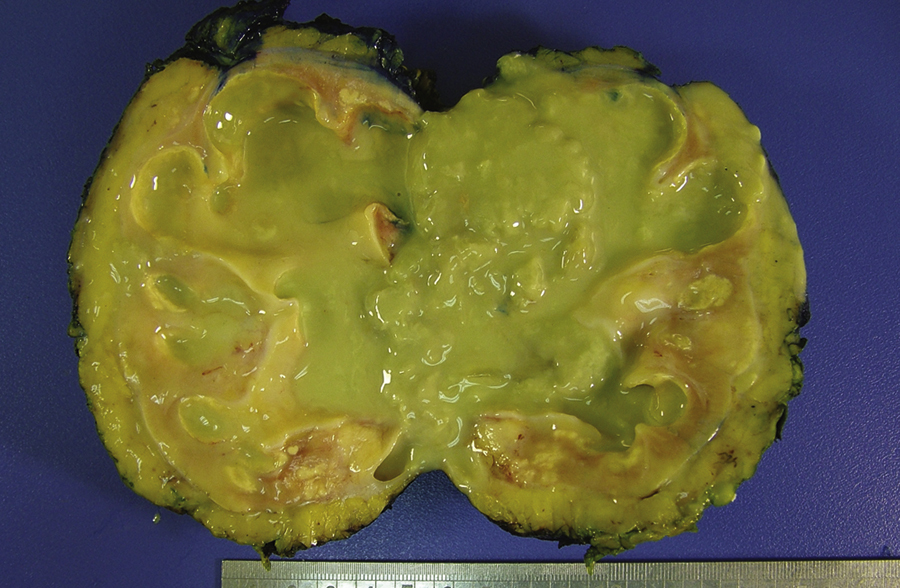
pyelonephritis /pī′əlōnəfrī″tis/ [Gk, pyelos + nephros, kidney, itis, inflammation] , a diffuse pyogenic infection of the pelvis and parenchyma of the kidney. Acute pyelonephritis usually results from an infection that ascends from the lower urinary tract to the kidney. Escherichia coli contamination of the urethral meatus is a common cause in females. Infection may spread to the kidney from other locations in the body. The onset of acute pyelonephritis is rapid and characterized by fever, chills, pain in the flank, nausea, and urinary frequency. Urinalysis reveals the presence of bacteria and white blood cells (WBCs). Antimicrobial treatment is continued for 10 days to 2 weeks. Relapse or reinfection is common. Chronic pyelonephritis develops slowly after bacterial infection of the kidney and may progress to renal failure. Most cases are associated with some form of obstruction, such as a stone or a stricture of the ureter. Treatment includes removal of the cause of obstruction and long-term antimicrobial therapy. ▪ OBSERVATIONS: The onset of symptoms is fairly rapid and is characterized by dull, constant flank pain, chills, and fever. Concomitant signs of a lower urinary tract infection (e.g., urinary frequency and dysuria) occur in about one third of individuals. Clinical symptoms are confirmed by urinalysis, which shows antibody-coated bacteria, bacteriuria, WBC casts, and pyuria; a CBC shows an increase in WBCs. Renal function studies may assist in the diagnosis of chronic disease. The most common complication of acute disease is septic shock and/or chronic pyelonephritis. With chronic disease, there is a 2% to 3% chance of developing end-stage renal failure. ▪ INTERVENTIONS: Oral or parenteral antiinfective drugs are used to combat infection. Continuous suppression antiinfective therapy may be used to treat recurrent or chronic infection. Antipyretics are used for fever. Hydration is managed by forcing oral fluids or using IV fluids for those unable to take in adequate oral fluids. Follow-up urine cultures are used to track effectiveness of antiinfective drugs. Surgery is used to drain large collections of pus and to correct underlying obstructions. Placement of a nephrostomy tube may be necessary to promote drainage of urine. ▪ PATIENT CARE CONSIDERATIONS: Key nursing goals for acute pyelonephritis are to reduce fever, relieve pain, promote comfort, and prevent complications. Individuals should be encouraged to drink at least 8 glasses of fluids daily even after acute infection subsides. Input and output should be closely monitored and urine should be checked for frequency, consistency, color, and odor. Rest is indicated to reduce fatigue, increase comfort, and allow the body to combat the infection. Education is aimed at teaching the individual about the disease, with a focus on the necessity to continue the full course of antibiotic therapy and to get follow-up urine cultures to ensure that infection is gone. Instruction is also necessary in preventing infection (cleansing perineum, proper wiping technique, adequate fluid intake, and cleansing after sexual activity) and in recognizing and treating early signs of urinary tract infection.