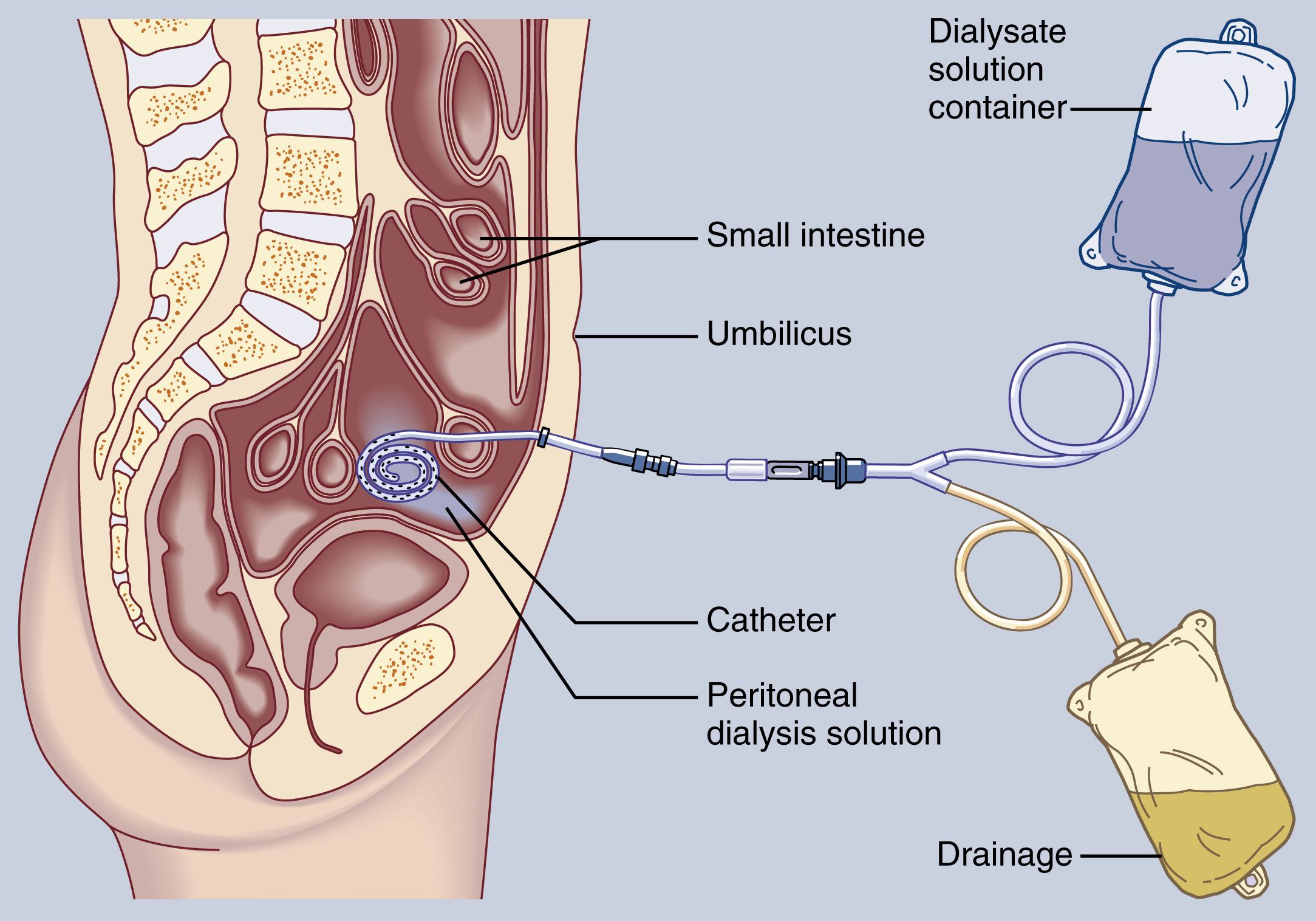
peritoneal dialysis (PD), a dialysis procedure performed to correct an imbalance of fluid or of electrolytes in the blood or to remove toxins, drugs, or other wastes normally excreted by the kidney. The peritoneum is used as a diffusible membrane. Peritoneal dialysis may be performed nightly for chronically ill children while they sleep and also may be carried out regularly at home. It is contraindicated in patients with extensive intraabdominal adhesions, localized peritoneal infection, and gangrenous or perforated bowels, although peritonitis may itself sometimes be treated by peritoneal lavage and antibiotics administered during peritoneal dialysis. ▪ METHOD: Under local anesthesia a many-eyed catheter is sutured in place in the peritoneum and a sterile dressing is applied. The catheter is connected to the inflow and outflow tubing with a Y connector, and the air in the tubing is displaced by the dialysate to prevent introduction of air into the peritoneal cavity. The amount and the kind of dialysate and the length of time for each exchange cycle vary with the age, size, and condition of the patient. There are three phases in each cycle. During inflow the dialysate is introduced into the peritoneal cavity. During equilibration (swell) the dialysate remains in the peritoneal cavity. By means of osmosis, diffusion, and filtration, the needed electrolytes pass via the vascular peritoneum to the blood vessels of the abdominal cavity, and the waste products pass from the blood vessels through the vascular peritoneum into the dialysate. During the third phase (drain) the dialysate is allowed to drain from the peritoneal cavity by gravity. ▪ INTERVENTIONS: The fluid is warmed to body temperature before instillation, and heparin, antibiotics, or other substances may be added to the dialysate. The patient’s fluid balance, respirations, pulse, blood pressure, temperature, and mental state are frequently evaluated, and blood glucose and electrolyte levels are tested regularly. The amount of fluid instilled and the amount and character of the fluid drained are noted. Bacteriological cultures of the drainage are performed regularly. A low-sodium, high-carbohydrate, high-fat 20- to 40-g protein diet is usually offered. Medication for pain may be necessary. Much peritoneal dialysis is now done in the home, not in facility. VNA referral is done for appropriate teaching and assessment with follow-up in dialysis centers. The need for dialysis and the techniques, dangers, and advantages of peritoneal dialysis are explained to the patient and the family. ▪ OUTCOME CRITERIA: Peritoneal dialysis may result in several complications, including perforation of the bowel, peritonitis, atelectasis, pneumonia, pulmonary edema, hyperglycemia, hypovolemia, hypervolemia, and adhesions. Peritonitis, the most common problem, is usually caused by failure to use aseptic technique and is characterized by fever, cloudy dialysate, leukocytosis, and abdominal discomfort. Dialysis may usually be continued while the infection is treated with antibiotics, which are given systemically or intraperitoneally. Atelectasis and pneumonia may result from compression of the thoracic cavity, with decreased respiratory excursion and blood flow to the bases of the lungs caused by an excessive volume of dialysate in the peritoneal cavity. Dyspnea, tachypnea, rales, and tachycardia require reevaluating the amount of dialysate, raising the head of the bed, and administering respiratory therapy to prevent atelectasis and pneumonia. Because patients with diabetes are at risk of developing hyperglycemia, serum and urine glucose levels are monitored, and, if necessary, sorbitol may be substituted for glucose in the dialysate. If dialysate fluid is retained in the peritoneal cavity, hypervolemia may occur, predisposing the patient to pulmonary edema and congestive heart failure. If the dialysate is removed too rapidly or if the dialysate used is a hypotonic glucose solution, hypovolemia may result. Adhesions often develop as a result of local irritation to the surrounding tissues caused by the intraperitoneal catheter.