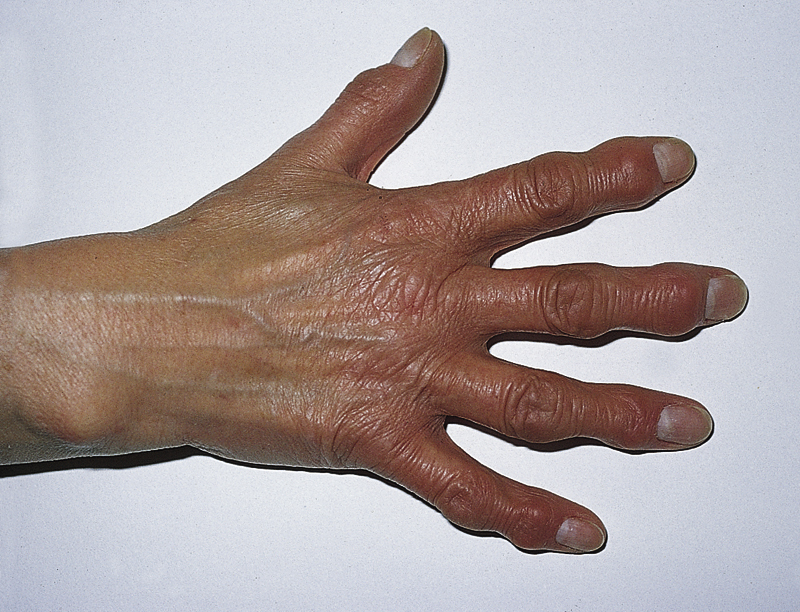
osteoarthritis /os′tē·ō′ärthrī″tis/ [Gk, osteon + arthron, joint, itis, inflammation] , a form of arthritis in which one or many joints undergo degenerative changes, including subchondral bony sclerosis, loss of articular cartilage, and proliferation of bone spurs (osteophytes) and cartilage in the joint. Inflammation of the synovial membrane of the joint is common late in the disease. Osteoarthritis is the most common form of arthritis. Its cause is unknown but may include chemical, mechanical, genetic, metabolic, and endocrine factors. Emotional stress often aggravates the condition. The disease usually begins with pain after exercise or use of the joint. Stiffness, tenderness to the touch, crepitus, and enlargement develop. Deformity, incomplete dislocation, and synovial effusion may eventually occur. Involvement of the hip, knee, or spine causes more disability than osteoarthritis of other areas. Treatment includes rest of the involved joints; use of a cane, a walker, or crutches to decrease weight-bearing; heat; and antiinflammatory drugs. Overweight patients may be advised to lose weight. Systemic corticosteroids are contraindicated, but intraarticular injections of corticosteroids may give relief. Surgical treatment is sometimes necessary and may reduce pain and greatly improve the function of a joint. Hip replacement, joint debridement, fusion, and decompression laminectomy are some of the surgical procedures used in treating advanced osteoarthritis. Also called degenerative joint disease. Compare rheumatoid arthritis. ▪ OBSERVATIONS: Early symptoms include deep, aching joint pain that is aggravated by exercise and that worsens as the day progresses. Inactivity contributes to stiffness. Midcourse of the disease is marked by reduced joint motion, tenderness, crepitus, grating sensation, flexion contractures, and joint enlargement. Manifestations late in the disease include tenderness on palpation, pain with passive ROM, increase in degree and duration of pain, joint deformity, and subluxation. Diagnosis is made by using clinical exam, with presence of usual manifestations plus possible Heberden’s or Bouchard’s nodes of the finger joints. Gait analysis may reveal altered motion patterns. Radiology may reveal narrowed joint space, increased density of subchondral bone, pseudocysts in subchondral marrow, and/or osteophytes at joint periphery. Analysis of synovial fluid typically shows high viscosity fluid that is yellow or transparent in color. Cultures of fluid are negative; WBC count is 200 to 2000/μL, with less than 25 polymorphonuclear leukocytes. Osteoarthritis of the spine can cause compression of the spinal cord, leading to weakness in the extremities, incontinence of bowel and bladder, and impotence. ▪ INTERVENTIONS: Treatment is aimed at pain reduction, slowing the degenerative process, and increasing joint mobility. Oral analgesics are used for pain; NSAIDs are used for inflammation; muscle relaxants and intraarticular steroid injections provide some transient relief. Topical agents (capsaicin) may provide temporary pain relief. Dietary supplements glucosamine and chondroitin sulfate are used for pain relief and improving joint mobility. Arthroscopy, osteotomy, laminectomy, fusion, and/or total joint replacement may be considered if conservative therapy fails. ▪ PATIENT CARE CONSIDERATIONS: Goals of the health care team include pain management, maintenance of joint function, and increasing activity tolerance and maintaining independence in self-care activities. Pain management makes use of a combination of pharmacological (analgesics, muscle relaxants, and steroids) and nonpharmacological (moist heat, massage, and rest) methods. Joint function is maintained by a judicious balance of rest and activity and use of a regular exercise program (isometric, isotonic, isokinetic, strengthening, stretching, ROM, and balance exercises). Joint protection measures, such as losing weight to reduce joint load, using assistive devices to aid mobility, avoiding forceful or repetitive movement, using good body mechanics and erect posture, and developing pacing techniques for daily routines can improve activity tolerance. Joint stability can be enhanced by actions such as avoiding soft chairs, using recliners, and placing pillows under knees; wearing sturdy, low-heeled shoes; removing environmental hazards; and using mobility aids and joint support devices. Decreasing pain and increasing joint flexibility lead to prolonged ability to perform activities of daily living.