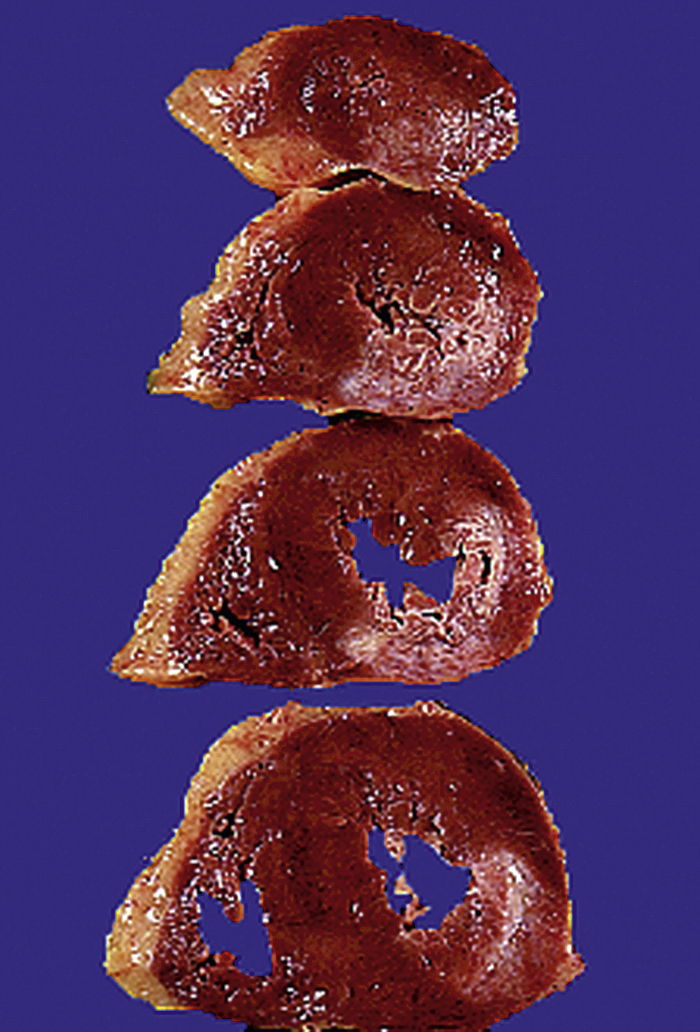
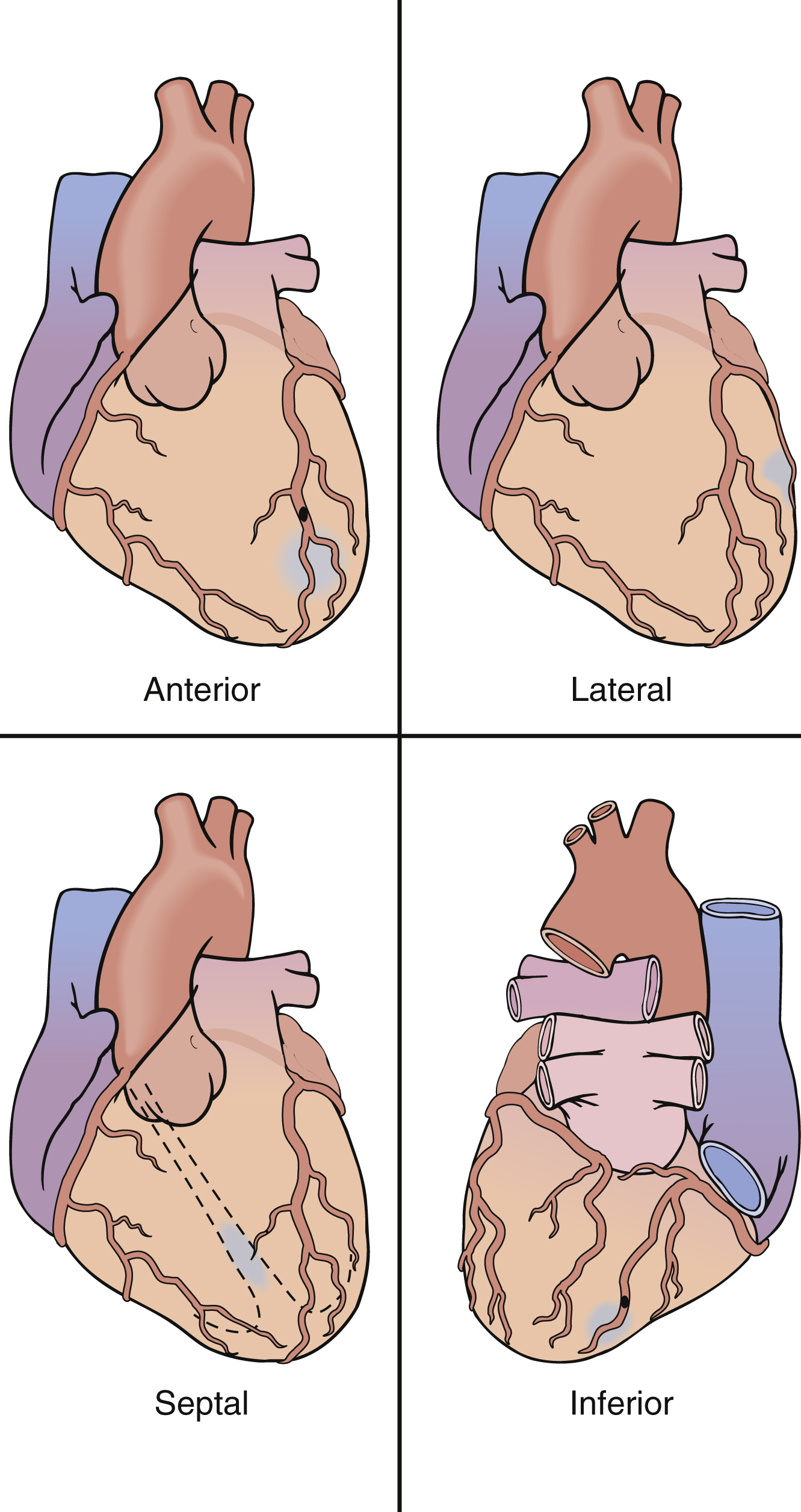
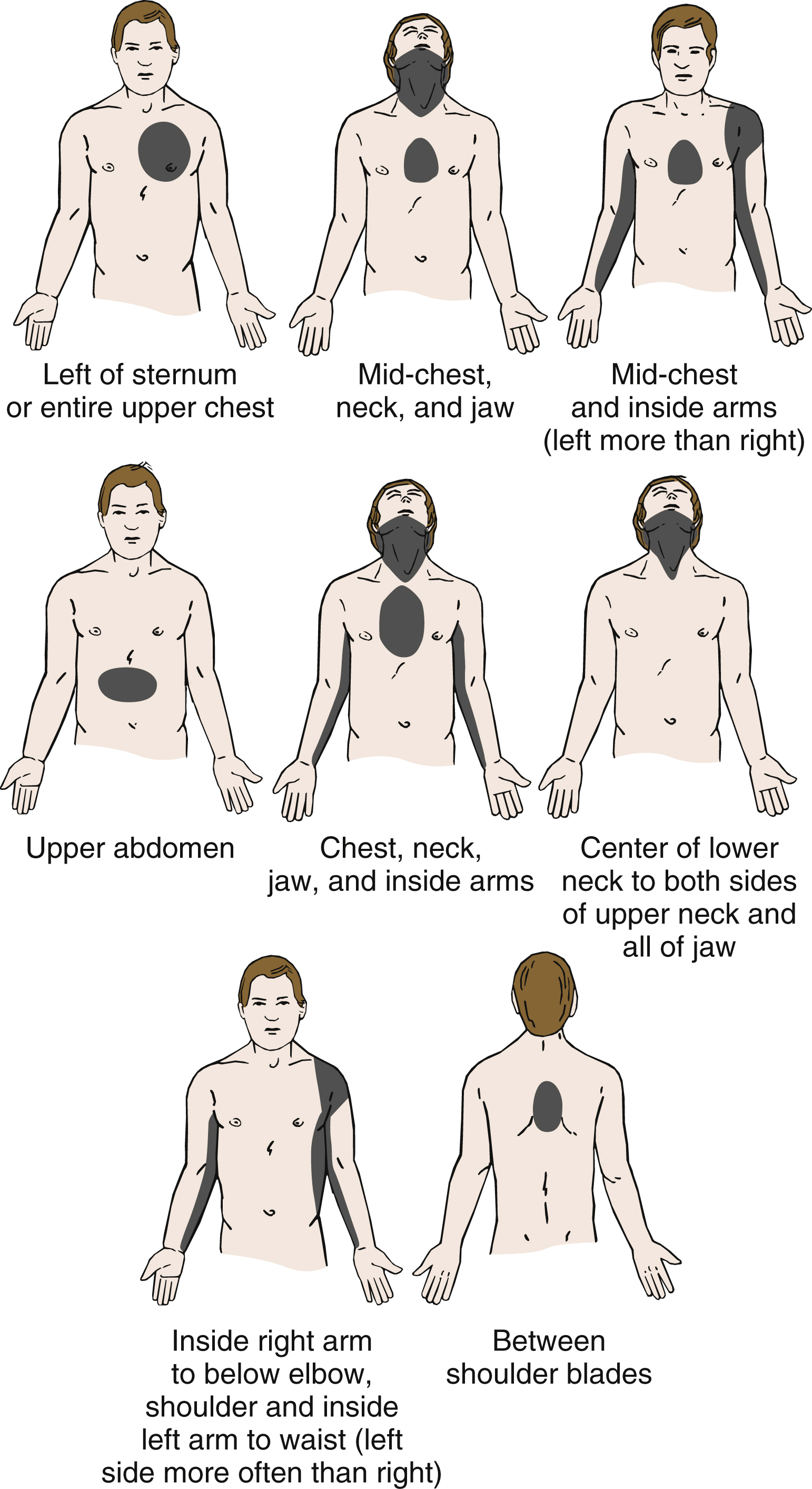
myocardial infarction (MI) /mī′ōkär″dē·əl/ [Gk, mys, muscle, kardia, heart; L, infarcire, to stuff] , necrosis of a portion of cardiac muscle caused by an obstruction in a coronary artery resulting from atherosclerosis, a thrombus, or a spasm. Also called heart attack. See also acute myocardial infarction. ▪ OBSERVATIONS: The onset of MI is characterized by a crushing, viselike chest pain that may radiate to the left arm, neck, jaw, or epigastrium and sometimes stimulates the sensation of acute indigestion or a gallbladder attack. The patient usually becomes ashen, clammy, short of breath, nauseated, faint, and anxious and often feels that death is imminent. Typical signs are tachycardia, a barely palpable pulse, low blood pressure, mildly elevated temperature, cardiac arrhythmia, and elevation of the S-T segment and Q wave on the electrocardiogram. Laboratory studies usually show an increased sedimentation rate, leukocytosis, and elevated serum levels of creatine kinase and its isoenzyme MB, lactic dehydrogenase and its isoenzymes, and glutamic-oxaloacetic transaminase. Potential complications in MI are pulmonary or systemic embolism, pulmonary edema, acute congestive heart failure, shock, ventricular tachycardia, ventricular fibrillation, and cardiac arrest. ▪ INTERVENTIONS: Emergency treatment of MI may require cardiopulmonary resuscitation before the patient reaches the hospital emergency department. Early IV administration of thrombolytic drugs and heparin improves left ventricular function, limits damage, and increases survival rates. Primary percutaneous transvenous coronary angioplasty (PTCA) is being used with increasing frequency and can achieve prompt reperfusion and help prevent the hemorrhagic risks of thrombolysis. Primary PTCA requires a well-staffed, well-equipped cardiac catheterization laboratory that can mobilize within 1 hour and achieve reperfusion within 2 hours. ▪ PATIENT CARE CONSIDERATIONS: The patient is admitted to an intensive care unit with continual electrocardiographic monitoring at the acute onset. Blood pressure, temperature, respiration, and apical pulse are checked frequently. Parenteral fluids may be administered, and the patient is usually served a low-sodium, low-cholesterol, low-fat diet. Stool softeners and laxatives may be indicated to prevent straining. The nurse’s role in helping the patient and family understand the nature and treatment of the disease is extremely important. Before discharge members of the health care team usually discuss the need to adhere to the prescribed diet and medication, to limit activities, to rest at regular periods, and to avoid caffeine, nicotine, large meals, and emotional stress. A cardiac rehabilitation program is often indicated and can play a major role in improving long-term health.