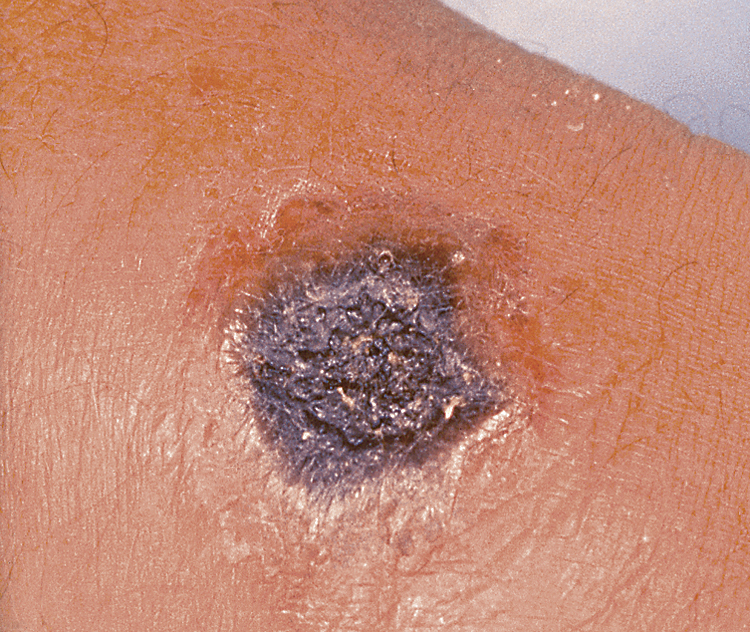
anthrax /an″thraks/ [Gk, anthrax, coal, carbuncle] , an acute infectious disease (reportable to public health officials) caused by the spore-forming bacterium Bacillus anthracis and occurring most frequently in herbivores (cattle, goats, sheep). Humans can become infected through skin contact, ingestion, or inspiration of spores from infected animals or animal products. Person-to-person transmission of inhalational disease does not occur. Anthrax in animals is usually fatal. Inspiration causes the most serious form in humans and is usually fatal, but in 95% of the cases it is acquired when a break in the skin has direct contact with infected animals and their hides. The cutaneous form begins with itching and then a 1- to 3-cm reddish-brown lesion that ulcerates and then forms dark eschar surrounded by brawny edema; the signs and symptoms that follow include internal hemorrhage, muscle pain, headache, fever, nausea, and vomiting. The pulmonary form, called woolsorter’s disease, is often fatal unless treated early. Early symptoms include low-grade fever, nonproductive cough, malaise, fatigue, myalgia, profound sweating, and chest discomfort. Later symptoms include an abrupt onset of a high fever and severe respiratory distress (cyanosis, dyspnea, stridor). Treatment is a 60-day course of antibiotics such as ciprofloxacin, levofloxacin, doxycycline, and penicillin. Contaminated surfaces should be cleaned with a 5% hypochlorite solution. A vaccine is available for veterinarians and for others for whom anthrax is an occupational hazard. The incubation period for anthrax is 7 to 42 days. Anthrax is an important potential bioterrorism agent. Also called malignant edema, malignant pustule, ragpicker disease. ▪ OBSERVATIONS: Cutaneous anthrax begins as an itchy, raised, red-brown skin bump, which develops into a vesicle and then a painless ulcer with a depressed black necrotic center. Lymph nodes in the adjacent area may be swollen and there may be fever, fatigue, and headache. Eschar from the ulcer dries and drops off with little or no scarring after 1 to 2 weeks. Cutaneous forms respond readily to treatment, but 20% of untreated cases result in death. Inhalation anthrax starts with a brief prodrome that resembles a viral respiratory illness followed by hypoxia, dyspnea, fever, muscle aches, headaches, and fatigue. Once the spores travel to the lymphatic system, respiratory failure and shock occur and death usually ensues regardless of treatment. Gastrointestinal anthrax presents with severe abdominal pain, fever, fatigue, anorexia, hematemesis, and bloody diarrhea. In some cases there may be lesions in the nose, mouth, and throat. The disease spreads systemically and is fatal in 30% to 60% of cases if not treated immediately. Diagnosis in all forms is made by history of possible exposure; by physical exam for presenting symptomatology and by isolation of Bacillus anthracis in blood, skin lesions, or respiratory secretions. Serological testing with enzyme-linked immunosorbent assay can confirm diagnosis. An anthracis test (available in specialized labs) can be used to detect anthrax cell-mediated immunity. Chest x-rays may detect mediastinal widening, pleural effusion, and infiltrates in inhalation anthrax. ▪ INTERVENTIONS: Antiinfectives, such as penicillin, doxycycline, Cipro, and/or Floxin, are the primary treatment. IV hydration and ventilator support are used for the inhalation form. Local and state authorities need to be notified in all suspected cases. Use of the anthrax vaccine is recommended in limited use for those at risk (e.g., military personnel, veterinarians, and livestock handlers). Side effects are high, and the schedule is six doses over an 18-month period. Treatment for exposure is usually a postexposure anthrax vaccine and a 60-day course of antibiotics. ▪ PATIENT CARE CONSIDERATIONS: Nursing care for inhalation anthrax is largely supportive and centers on management of airway and mechanical ventilation, fluid management, and comfort measures. Every member of the health care team should be prepared for an effective response should anthrax be used in a bioterrorism event. This includes familiarization with workplace policies, procedures, and protocols, and maintenance of current knowledge regarding bioterrorism threats.