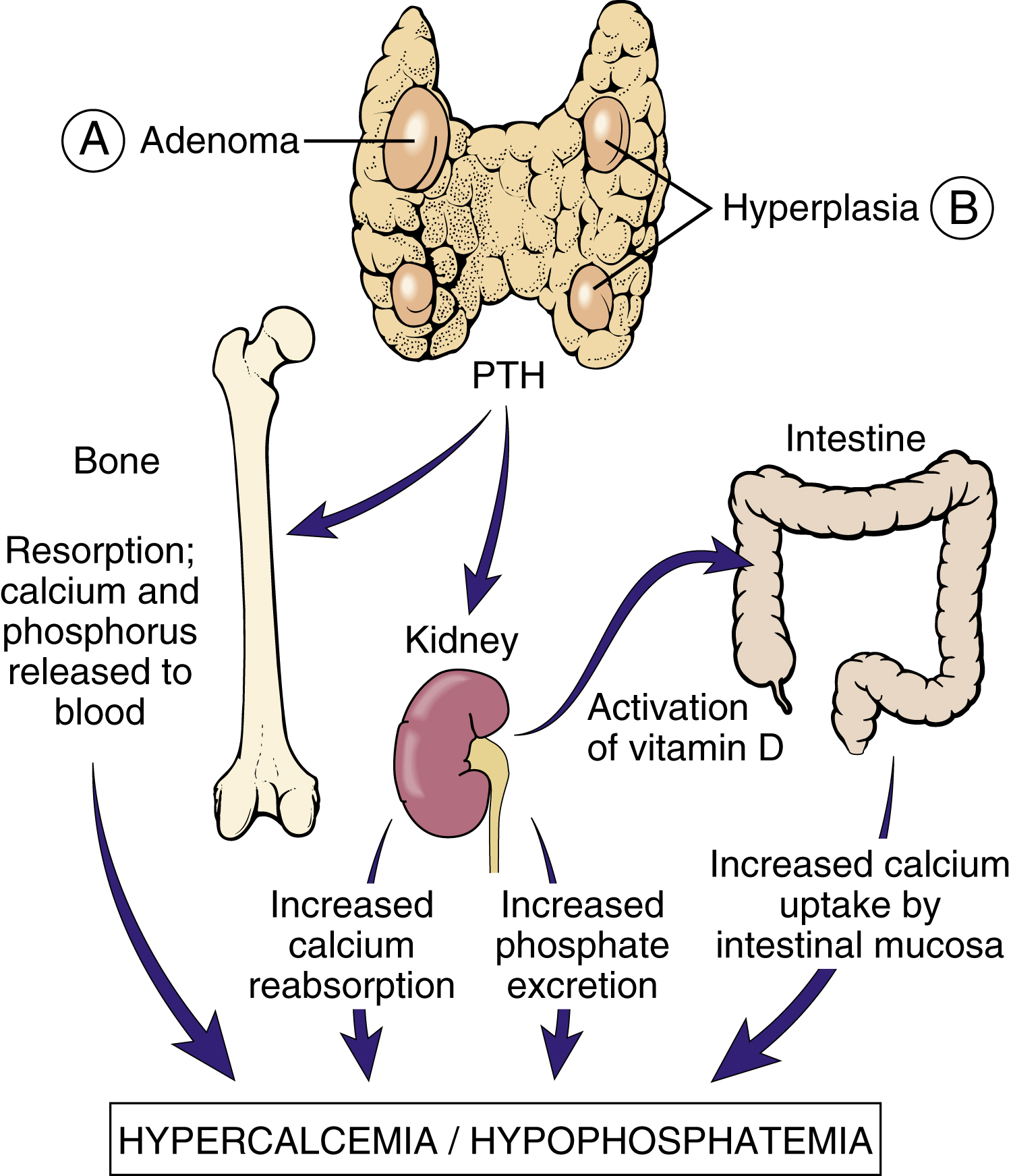
hyperparathyroidism /-per′əthī″roidiz′əm/ [Gk, hyper + para, beside, thyreos, shield, eidos, form] , an abnormal endocrine condition characterized by hyperactivity of any of the four parathyroid glands with excessive secretion of parathyroid hormone (PTH), which causes increased resorption of calcium from the skeletal system and increased absorption of calcium by the kidneys and GI system. The condition may be primary, originating in one or more of the parathyroid glands and usually caused by an adenoma, or secondary, resulting from an abnormal hypocalcemia-producing condition in another part of the body, which causes a compensatory hyperactivity of the parathyroid glands. ▪ OBSERVATIONS: Hypercalcemia in primary hyperparathyroidism results in dysfunction of many body systems. In the kidneys, tissue calcifies, calculi form, and renal failure may ensue. In addition, excess phosphorus is excreted, and excess 1,25 (OH)2 D (vitamin D) is synthesized. In the bones and joints, osteoporosis develops, causing pain and fragility; fractures, synovitis, and pseudogout often occur. In the GI tract, chronic, piercing epigastric pain may develop as a result of pancreatitis and increased gastrin production; anorexia and nausea may occur; and vomiting of blood may result if peptic ulceration occurs. In the neuromuscular system, generalized weakness and atrophy develop if the condition is not corrected, and changes in the central nervous system produce alteration of consciousness, coma, psychosis, abnormal behavior, and disturbances of personality. Secondary hyperparathyroidism may result in many of these signs of calcium imbalance and in various abnormalities of the long bones, such as rickets. The diagnosis of primary hyperparathyroidism is made by laboratory findings of increased levels of PTH and calcium in the blood and by the characteristic appearance of the bones on radiographic films. Calcium in the blood and urine and chloride and alkaline phosphatase in the blood are present in excessive amounts; phosphorus is present in the serum in less than normal amounts. ▪ INTERVENTIONS: Primary parathyroidism that is the result of an adenoma of one of the glands is treated by excision of the tumor; other causes of primary disease may require excision of up to one half of the glandular tissue. In asymptomatic patients over 50, noninterventional observation may be indicated. Dietary intake of calcium may be limited, and adequate hydration must be maintained. Estrogens may be used in postmenopausal females. Bisphosphates may be administered in severe hypercalcemia to lower the serum calcium level. After surgery, calcium levels in the blood may drop rapidly to dangerously low levels if frequent laboratory evaluations are not made and supplemental calcium is not given as required. Secondary hyperparathyroidism is managed by treating the underlying cause of hypertrophy of the gland. Vitamin D is frequently given, and peritoneal dialysis may be necessary to remove excess calcium from the circulation. ▪ PATIENT CARE CONSIDERATIONS: Frequent laboratory evaluations of blood levels of calcium, phosphorus, potassium, and magnesium are necessary throughout the course of treatment. Because fractures occur easily and are common, great care is taken to prevent trauma to the patient. IV hydration is usually performed to dilute the concentration of calcium, and the lungs are assessed regularly to detect pulmonary edema in its earliest stages. Tetany is a warning sign of severe hypoglycemia; calcium gluconate is kept available for immediate use after surgery. Walking and moving about cause pain but accelerate healing of the affected bones and are therefore encouraged.