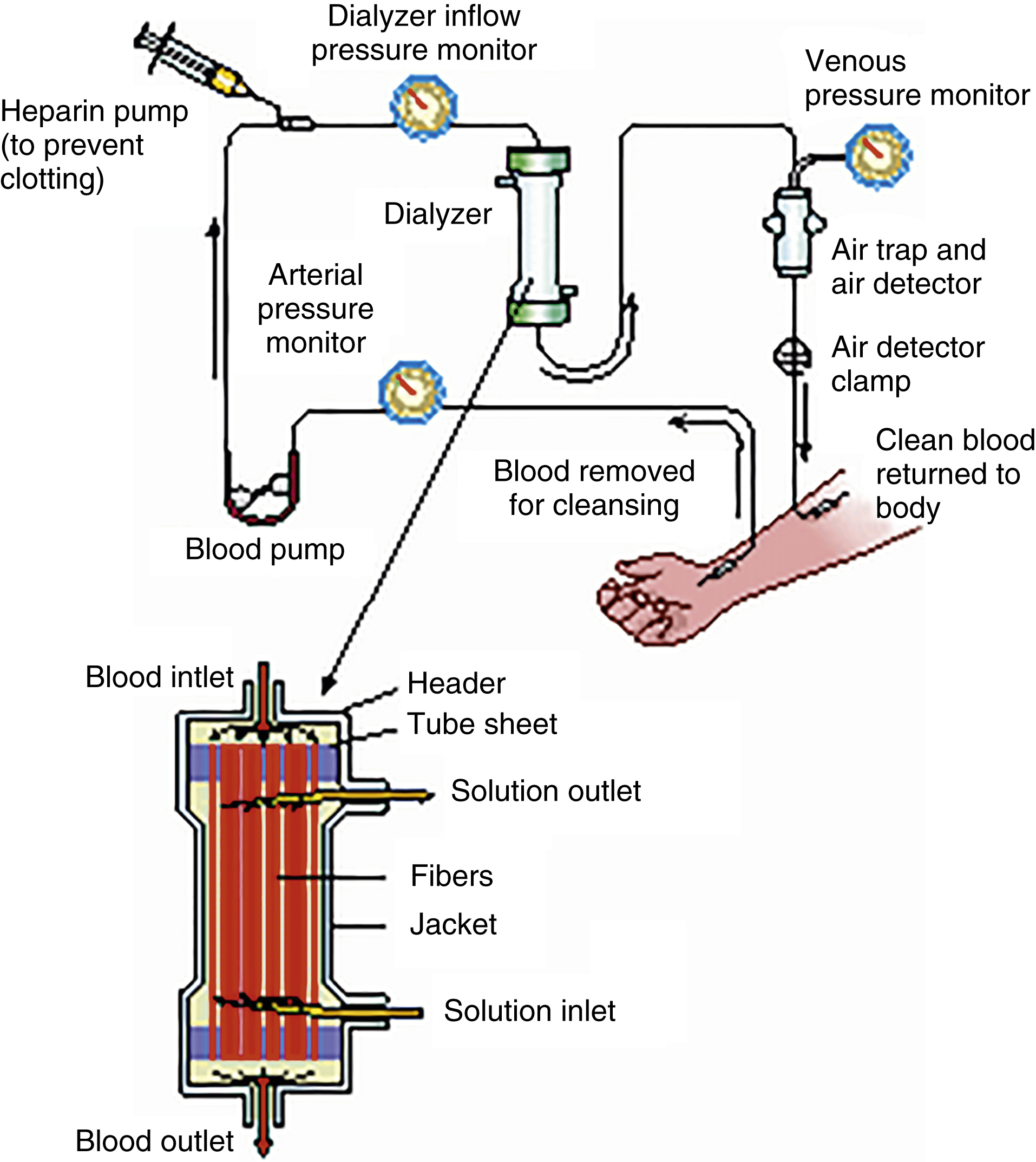
hemodialysis /hē′mōdī·al″isis, hem′-/ [Gk, haima + dia, apart, lysis, loosening] , a procedure in which impurities or wastes are removed from the blood, used in treating patients with renal failure and various toxic conditions. The patient’s blood is shunted from the body through a machine for diffusion and ultrafiltration and then returned to the patient’s circulation. Hemodialysis requires access to the patient’s bloodstream, a mechanism for the transport of the blood to and from the dialyzer, and a dialyzer. Also spelled haemodialysis. See arteriovenous fistula, def. 2, external shunt. ▪ METHOD: Access may be achieved by an external shunt or an arteriovenous fistula. When hemodialysis is being performed, cannulas are separated, allowing the arterial blood to flow to the dialyzer and the dialyzed blood to return from the dialyzer to the circulation through the cannula in the vein. An arteriovenous fistula is created by the anastomosis of a large vein to an artery. Large-bore needles are threaded into superficial vessels enlarged by the increased flow caused by the fistula. Various dialyzers may be used. Hemodialysis takes from 3 to 8 hours depending on the patient’s condition, weight, and laboratory values and may be necessary daily in acute conditions or two to three times a week in chronic renal failure. ▪ INTERVENTIONS: A decrease in blood flow through the shunt may cause clotting. Therefore, any factor that may result in a slowing of the flow should be avoided. Some of these factors are systemic hypotension, infection of the shunt or fistula, compression of the shunt or fistula, thrombophlebitis, and prolonged inflation of a blood pressure cuff. Infection is prevented in the area around an external shunt by placing a sterile dressing over the shunt and changing the dressing daily. Before the procedure is begun, the patient is told how long it will take, what pain or discomfort may be expected, what will be felt afterward, what food or activity will be allowed during the procedure, and whether family or friends may be present during treatment. Headache, nausea, and muscle cramps are common, especially during the procedure and for a few hours afterward. The patient usually feels best on the day after hemodialysis. Rest, an antiemetic, and a mild analgesic may make the procedure more comfortable. Most patients need emotional support and some physical assistance during hemodialysis. The physical status of the patient is monitored frequently throughout. Blood pressure, pulse, and blood tests for electrolyte and acid-base balance are performed. Normal saline solution may be administered to counteract hypotension that results from rapid removal of fluid from the intravascular compartment. The patient is weighed before and after the treatment to determine the amount of fluid lost during the procedure. An anticoagulant is usually given to prevent coagulation of the blood in the dialyzer, cannulas, or catheters. To prevent hemorrhage, protamine sulfate may be administered after the procedure to reverse the effect of the anticoagulant. Any treatment that causes tissue trauma, such as dental extraction, venipuncture, or intramuscular injection, is not recommended during or immediately after dialysis. ▪ OUTCOME CRITERIA: The discomfort before, during, and just after dialysis; the prolonged time of relative immobility during the procedure; and the dietary restrictions necessary in renal insufficiency all cause considerable stress in the patient. Adjustments in the patterns of daily life are necessary and require the assistance of professionals with experience and training.