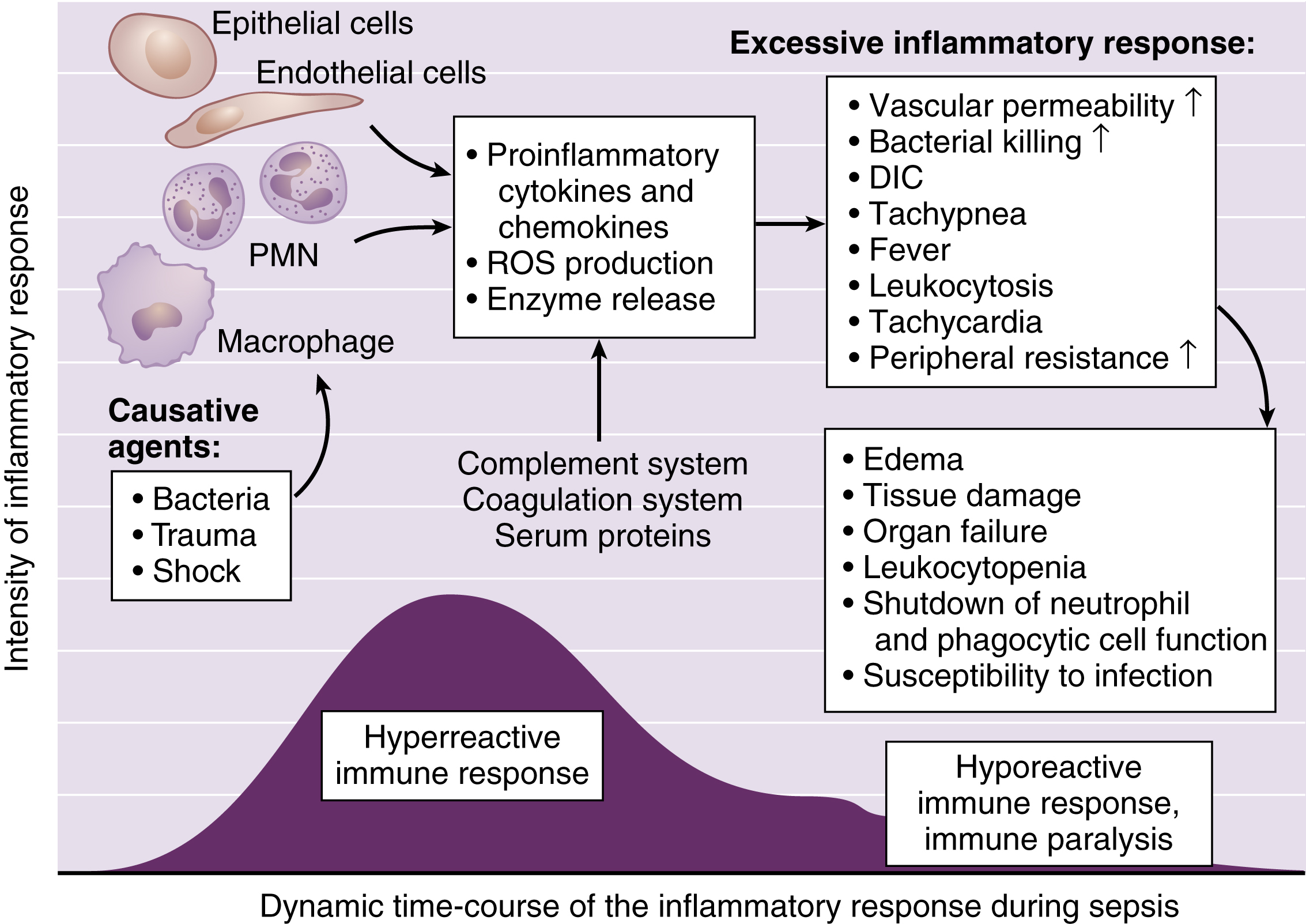
disseminated intravascular coagulation (DIC) [L, dis + seminare, to sow, intra, within, vasculum, little vessel, coagulare, to curdle] , a grave coagulopathy resulting from the activation of clotting and anticlotting processes in response to disease or injury, such as septicemia, acute shock, poisonous snakebites, neoplasms, obstetric emergencies, severe trauma, extensive surgery, and hemorrhage. The primary disorder initiates generalized intravascular clotting, which in turn activates fibrinolytic mechanisms. As a result, the initial hypercoagulability is succeeded by a deficiency in clotting factors with coagulopathy and hemorrhaging. Also called consumption coagulopathy, defibrination syndrome. ▪ OBSERVATIONS: Purpura on the lower extremities and abdomen, reflecting fibrin deposits in capillaries, is a common first sign of DIC. Hemorrhagic bullae, cyanosis of the extremities, and focal gangrene in the skin and mucous membranes may follow. Hemorrhages from incisions or catheter or injection sites, GI bleeding, hematuria, pulmonary edema, pulmonary embolism, progressive hypotension, tachycardia, absence of peripheral pulses, restlessness, convulsions, or coma may occur. Laboratory studies generally show a marked deficiency of blood platelets, low levels of fibrinogen and other clotting factors, prolonged prothrombin and partial thromboplastin times, and abnormal erythrocyte morphological characteristics. ▪ PATIENT CARE CONSIDERATIONS: The management of acute and chronic forms of disseminated intravascular coagulation (DIC) should primarily be directed at treatment of the underlying disorder. The care of a patient with life-threatening DIC requires careful monitoring, observation for evidence of bleeding, extremely gentle handling, maintenance of a safe environment, and emotional support.