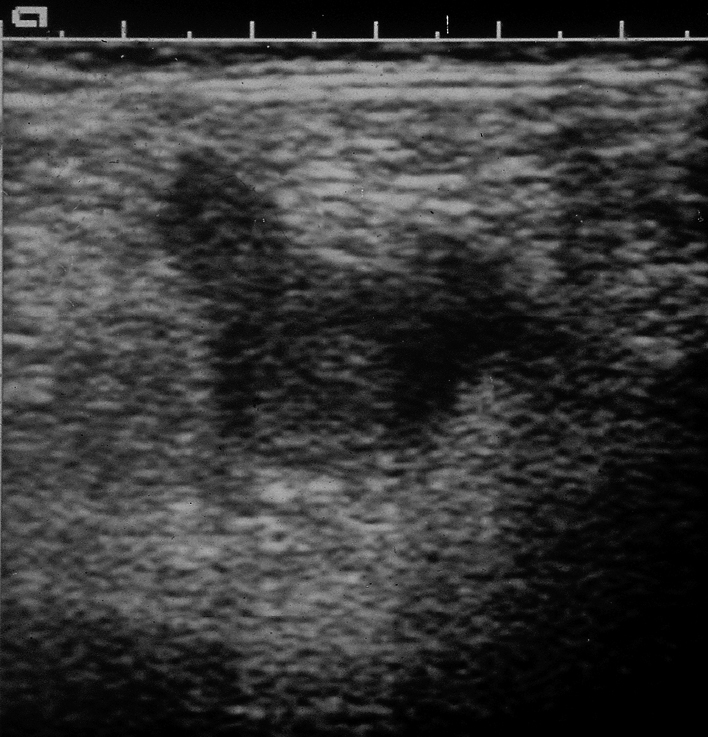
deep vein thrombosis (DVT), a disorder involving a thrombus in one of the deep veins of the body, most commonly the iliac or femoral vein. Symptoms include tenderness, pain, swelling, warmth, and discoloration of the skin. A deep vein thrombus is potentially life threatening. Treatment includes the use of thrombolytic and anticoagulant drugs and interventional radiology. Treatment goals are directed to prevention of movement of the thrombus toward the lungs. See also pulmonary embolism. ▪ OBSERVATIONS: It may be asymptomatic or manifest as tenderness, pain, warmth, and swelling in the affected extremity with deep reddish or blue color. There is a positive Homans’ sign in about 10% of cases, which affects a lower extremity. Serial compression ultrasonography is the initial test used for diagnosis. Magnetic resonance direct thrombus imaging may be used for thrombi undetectable on ultrasound. Contrast venography remains the gold standard for detection of lower extremity DVT. Chronic venous insufficiency and pulmonary embolus are the most common complications of thrombosis. ▪ INTERVENTIONS: Initial treatment is heparin or enoxaparin followed by warfarin for maintenance treatment for 3 to 6 months. Continued monitoring of prothrombin time and partial thromboplastin time is done during anticoagulant therapy. Ligation, clipping, plication, and thrombectomy are surgical alternatives when thrombus fails to respond to anticoagulant therapy. An extravascular vena cava interruption with possible placement of intracaval filter is used for cases involving probable emboli. Analgesics are given for pain; however, aspirin is contraindicated because it interferes with platelet function. Enoxaparin may be used with patients at high risk for DVT to prevent thrombus formation. ▪ PATIENT CARE CONSIDERATIONS: The immediate focus of the health care team is on prevention of pulmonary emboli, pain relief, prevention of skin breakdown, and prevention of complications related to anticoagulant therapy. Bed rest is no longer recommended. Early ambulation is encouraged, and compression stockings may be prescribed to reduce pain and swelling. Individuals are closely observed for signs of bleeding (e.g., gums, nasal mucosa, stool, and urine). Safety precautions are instituted to prevent bruising while on anticoagulants and to prevent skin ulceration of affected extremity. Individuals are monitored for manifestations of pulmonary emboli, including sudden dyspnea, tachypnea, and pleuritic chest pain. Education is important and includes effects and side effects of anticoagulant therapy; need for ongoing blood tests to monitor clotting and regulate anticoagulant dosage; avoidance of activities that may precipitate bleeding; avoidance of anticoagulant over-the-counter medications that may interfere with clotting (e.g., aspirin/aspirin products, NSAIDs, and herbal products). Education is needed about signs of pulmonary embolus and the need for immediate medical attention should they occur. Instruction is provided to prevent pooled blood in the lower extremities, including regular use of compression garments and avoidance of prolonged standing, sitting, or walking. Teaching also includes prevention of future thrombosis episodes, such as avoidance or correction of modifiable risk factors (e.g., tobacco use or alcohol abuse, use of oral contraceptives or hormone replacement therapy, and prolonged periods of inactivity), regular exercise program, proper posture, and balanced diet with weight loss if indicated.