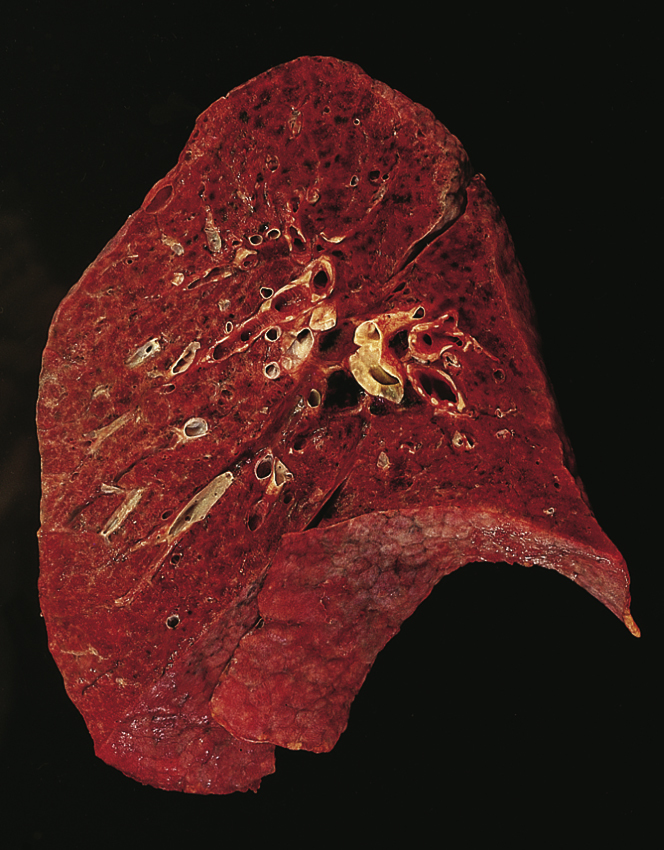
adult respiratory distress syndrome (ARDS), severe pulmonary congestion characterized by diffuse injury to alveolar-capillary membranes. Fulminating sepsis, especially when gram-negative bacteria are involved, is the most common cause. ARDS may occur after trauma; near-drowning; aspiration of gastric acid; paraquat ingestion; inhalation of corrosive chemicals, such as chlorine, ammonia, or phosgene; or the use of certain drugs, including barbiturates, chlordiazepoxide, heroin, methadone hydrochloride, propoxyphene hydrochloride, and salicylates. Other causes include diabetic ketoacidosis, fungal infections, high altitude, pancreatitis, tuberculosis, and uremia. Also called acute respiratory distress syndrome, congestive atelectasis, hemorrhagic lung, noncardiogenic pulmonary edema, pump lung, shock lung, stiff lung, wet lung, chronic obstructive pulmonary disease. ▪ OBSERVATIONS: Signs and symptoms include dyspnea, tachypnea, adventitious breath sounds, hypoxemia, and decreased lung compliance. Changes occurring within the lung include damage to the alveolar-capillary membranes, leakage of plasma proteins into the alveoli, dilution of surfactant, cessation of surfactant production, hemorrhage, interstitial edema, impaired gas exchange, and ventilation-perfusion defects. ▪ INTERVENTIONS: Treatment includes establishing an airway, administering oxygen, improving the underlying condition, removing the cause of ARDS, suctioning the respiratory passages as necessary, and reducing oxygen consumption. When ventilation cannot be maintained and there is evidence of a rising partial pressure of carbon dioxide in arterial blood, mechanical ventilation is necessary. Positive end-expiratory pressure (PEEP) is widely used in the treatment of ARDS. All interventions for ARDS are supportive; there is no cure. ▪ PATIENT CARE CONSIDERATIONS: The patient with ARDS requires constant and meticulous care, reassurance, and observation for changes in respiratory function and adequacy, including signs of hypercapnia, hypoxemia (especially confusion), skin flushing, and behavior changes such as agitation and restlessness. Increasing hypoxia may be signaled by tachycardia, elevated blood pressure, increased peripheral resistance, and fulminating respiratory failure. If PEEP is being used, the patient is carefully observed for a sudden disappearance of breath sounds accompanied by signs of respiratory distress—an indication that pneumothorax may be present. Respiratory therapy, sterile suction techniques, and position changes are continued as necessary. The patient’s weight is measured frequently, chest x-ray films are evaluated, and bacteriological cultures of secretions are analyzed for the causative organism. Throughout treatment, ventilation is carefully monitored through analysis of arterial blood gases. ARDS has a 50% mortality rate.